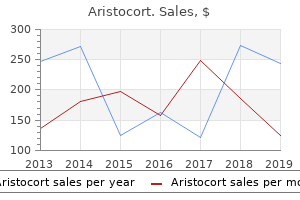
Aristocort"Generic aristocort 4 mg without prescription, allergy shots cause joint pain". By: W. Grim, M.A., Ph.D. Program Director, Marian University College of Osteopathic Medicine If the metastatic brain tumor is in the cerebellum or near the brainstem anatomy allergy shots lymphoma buy genuine aristocort, radiation has sometimes been dangerous in that it increases brain edema and intracranial pressures leading to signs of herniation. In addition, high dose steroids should be considered with the radiation to decrease edema. Moreover, the improved survival time in this patient population, due to treatment with new and improved chemotherapy drugs such as trastuzumab, may allow more time for brain metastases to develop and become clinically apparent. This type of therapeutic rationale that chooses a lipophilic drug with no history of efficacy in its primary tumor needs to be reconsidered by the treating oncologist. The same chemotherapy drug used for the primary tumor histology should be strongly considered for patients with metastatic brain lesions from the particular primary tumor, chemosensitive primary tumors, and progressive systemic disease. Melanoma is commonly considered to be an immunogenic cancer similar to renal cell cancer, and there have been great advancements in the field of immunotherapy to treat this disease. Again, we see that the treatment of brain metastases in melanoma appears to be based upon using agents known to have historical efficacy against primary melanoma. As a general rule for treating brain metastases, the agents of choice should be taken from those known to be efficacious in treating the primary tumor. Nevertheless, treatment of brain metastases should focus on using local therapies for palliating symptoms in addition to using chemotherapeutics and targeted agents with known efficacy against the primary tumor. We also want to thank Tyler Golato and Uri Hochfeld for assistance in the preparation of the chapter. Tamoxifen paradoxically decreases paclitaxel deposition into cerebrospinal fluid of brain tumor patients. Early changes in peritumorous oedema and contralateral white matter after dexamethasone: a study using proton magnetic resonance spectroscopy. Front-line paclitaxel/cisplatin-based chemotherapy in brain metastases from non-small-cell lung cancer. Hyaluronidase is more elevated in human brain metastases than in primary brain tumours. The importance of brain temperature in alterations of the blood-brain barrier following cerebral ischemia. Randomized study of tamoxifen deposition into human brain tumors: implications for the treatment of metastatic brain tumors. The effect of P-glycoprotein on paclitaxel brain and brain tumor distribution in mice. Practice parameter: anticonvulsant prophylaxis in patients with newly diagnosed brain tumors. Report of the quality standards subcommittee of the American Academy of Neurology. Predilection of brain metastasis in gray and white matter junction and vascular border zones. Modulation of the blood-brain barrier in oncology: therapeutic opportunities for the treatment of brain tumours Outwitting the blood-brain barrier for therapeutic purposes: osmotic opening and other means. Breast cancer resistance protein and P-glycoprotein limit sorafenib brain accumulation. Human epidermal growth factor receptor 2-positive breast cancer and central nervous system metastases. Distribution of tamoxifen and metabolites into brain tissue and brain metastases in breast cancer patients. Erlotinib efficacy and cerebrospinal fluid concentration in patients with lung adenocarcinoma developing leptomeningeal metastases during gefitinib therapy. Hypoxia-inducible factor-1 modulates gene expression in solid tumors and influences both angiogenesis and tumor growth. Prolonged stabilization of multiple and single brain metastases from breast cancer with tamoxifen. Incidence of brain metastases in a cohort of patients with carcinoma of the breast, colon, kidney, and lung and melanoma. The effect of dexamethasone on the uptake of cisplatin in 9L glioma and the area of brain around tumor. Mammalian heparanase: involvement in cancer metastasis, angiogenesis and normal development.
Pictures show embolus lodged near the origin of the superior mesenteric artery (red arrow) as well as ischemic loops of bowel allergy testing washington dc discount aristocort 4 mg line. Note poor contrast penetration inside the intestinal wall with reduced blood flow and dilatation of the small bowel loops (yellow arrow). Note the marked thickening of the wall of affected ileal loops with narrowing of the intestinal lumen (arrows). Note the extensive thickening of the wall of the small bowel loops with smooth serosal surfaces and appearance of rigidity caused by wall infiltration and organized edema and hemorrhage (arrows). There is marked edema of the mesentery (yellow arrow) in addition to the less specific thickening of the small bowel wall. Thumbprinting is most characteristic in the early stages but bulging tends to disappear later and turn into a flatter mucosal lesion. Marked thumbprinting is apparent at clinical presentation (a) but angiography (a) (b) features of each of these two conditions may help identify the respectively affected segments, as illustrated by the barium enema pictures shown here: diverticulitis (a) and ischemic colitis (b). Note the markedly thickened bowel wall with some air remaining in the lumen (arrows). Note the sharply different wall thickness between the affected transverse segment and the spared ascending colon and hepatic flexure (arrows). Radiographically they may be long, with tapered edges (a) and usually distinct from the sharper-edged neoplastic strictures (b). The pseudopolyps may potentially lead to confusion with late-stage inflammatory bowel disease. Note, on the barium enema picture (a), the characteristic long thumbprinting and narrowing of a segment of the descending colon and (b) the surgically resected specimen including a sigmoid carcinoma. There is luminal narrowing by a lobulated mass effect caused by edema and ulceration in the ischemic segment. However, distinction may be usually established by the pathologist through multiple morphological features. The histological appearance of lesions observed in tissue specimens is often characteristic of acute or delayed radiation injury. However, no individual histological feature is pathognomonic for radiation-induced damage. Therefore, histological findings may mimic other pathological conditions and must be interpreted carefully within the appropriate clinical context for a given patient. Patients may present with acute symptoms days or weeks after radiation therapy is initiated or with delayed clinical syndromes that may occur years after therapy. The early effects primarily involve the mucosa, which is lined by rapidly proliferating epithelial cells that are sensitive to the acute effects of radiation injury. Clinical symptoms include odynophagia, diarrhea, nausea, vomiting, or gastrointestinal bleeding; the symptoms depend on the location of the radiation field, the dose of irradiation, and the fractionation schedule. The delayed effects of therapeutic irradiation are more likely to present with chronic diarrhea, fibrosis, ulcer formation, or bleeding, and are thought to be secondary to damage to the vasculature of the organs involved. The histopathological features of acute radiation injury are dominated by evidence of acute injury to the mucosa. Apoptosis of lamina propria lymphocytes and epithelial cells and the cessation of epithelial cell replication occur within hours of a radiation dose. Mature, differentiated epithelial cells continue to be lost in the absence of replacement by replication of the progenitor cells within these epithelia, resulting in the subsequent loss of mucosal function. Mucosal and submucosal edema may also be observed within the radiation field as a result of endothelial dysfunction. Specimens from patients with acute hepatic injury secondary to therapeutic irradiation for solid neoplasms are rarely obtained. However, venoocclusive disease is not uncommon in bone marrow transplant patients following cytoreductive therapy with combined chemotherapy and irradiation. Onset of venoocclusive disease in this setting usually occurs before 5 weeks posttransplant. Changes in hepatic histology include vascular congestion that is most prominent in centrilobular areas, subendothelial edema, endothelial destruction, sinusoidal dilation, and centrizonal hepatocyte necrosis with attenuation of the hepatocellular cords.
The pancreas (P) is hyperechoic to the liver (L) and similar in echotexture to the retroperitoneal fat allergy forecast katy tx order aristocort with mastercard. Two hypoechoic eccentric rings are seen, denoting the bowel wall of the intussusceptum (arrowhead) and the intussuscipiens (arrow). The echogenic area between the two rings is the mesenteric fat (M) accompanying the intussusceptum into the intussuscipiens. Transverse image of the pancreas shows pancreatic ductal dilation (D), abruptly terminating in the pancreatic head secondary to an ill-defined hypoechoic mass (M). There is associated pancreatic atrophy as minimal parenchyma is seen surrounding the dilated pancreatic duct (arrowheads). Note that the superior part of the image does not show the usual anterior abdominal wall musculature, as the transducer was placed immediately over the pancreas. Ultrasound guidance can also be used during paracentesis and the percutaneous drainage of visualized fluid collections. Intraoperative ultrasound Ultrasound can be used within the operating room to detect masses for biopsy and resection. Types of echoendoscopes There are two major types of echoendoscopes: radial imaging and linear imaging. Case 1 A 57-year-old man with a history of reflux presents with 2 months of progressive dysphagia for solids more than liquids. The mass extends beyond the esophageal muscularis propria and invades the adjacent left pleura. Case 2 A 43-year-old man with history of cystic fibrosis presents with hemoccult positive stools and mild anemia. Case 4 A 47-year-old man with a history of gastroesophageal reflux undergoes upper endoscopy. Fine-needle aspiration demonstrates spindle-shaped cells that stain positive for C-kit protein. Other features (not shown) included calcifications and an echogenic pancreatic duct. Water (W) in the gastric lumen facilitates imaging of the wall layers that correspond to mucosa, submucosa, muscularis propria, and surrounding tissue. This instrument also has Doppler capability for demonstration of blood flow in these vessels. The wire was withdrawn from the duodenal bulb (yellow) and re-advanced in a retrograde fashion to facilitate transpapillary stent placement. The collection has a large amount of debris (asterisk) with a thin sliver of fluid (arrow). In addition to dramatically reducing motion and respiratory artifacts, this narrow temporal window has directly impacted protocol design, enabling the consistent acquisition of images at peak enhancement. This has proven particularly valuable in the imaging of traditionally hypervascular tumors such as hepatocellular carcinoma, pancreatic neuroendocrine tumor, and renal cell carcinoma, all of which are much better visualized when imaged during peak arterial enhancement. Following data acquisition, easy-to-use three-dimensional (3D) postprocessing software is now widely available and routinely utilized in practices across the country, allowing the radiologist to view the scan data in any imaging plane and utilize 3D techniques that can accentuate sites of pathology. The hollow viscera of the gastrointestinal tract Techniques Oral contrast Identifying abnormalities of the luminal gastrointestinal tract, whether neoplastic or inflammatory, relies on the ability to adequately visualize the bowel wall and gauge abnormalities in either bowel wall thickness or enhancement. In general, a complete evaluation of the bowel wall requires optimal distension of the bowel lumen with an enteric contrast agent. While quite useful in differentiating loops of bowel from adjacent structures, they are often associated with "beam-hardening" or streak artifacts that might limit optimal evaluation of the bowel wall (in terms of enhancement or thickening). The most commonly used neutral agents include water, methylcellulose agents, and commercially available products such as Volumen (E-Z-Em; Lake Success, New York), which has a density value slightly greater than water. Given that these agents do not result in beam hardening or streak artifact, while still producing very good distension of the bowel lumen, they are considered the best contrast agents for evaluating the bowel wall. Neutral agents are most commonly utilized in enterography protocols where evaluation of the bowel wall for subtle abnormal enhancement, thickening, or tumors is the goal of the study, as these agents allow excellent visualization of the enhancing wall that may otherwise be obscured by positive agents. In addition, when 3D postprocessing is performed, it is beneficial to use neutral contrast agents, as they allow 3D reconstructions of the vasculature without the need for extensive postprocessing to segment the bowel loops. Alternatively, when positive oral agents are used these "white" loops need to be manually removed using postprocessing, as they will otherwise obscure the adjacent contrast-enhanced vessels, particularly when maximum intensity projection reconstruction techniques are utilized. Intravenous contrast enhancement dramatically increases the conspicuity of pathological processes throughout the gastrointestinal tract, which in many cases may not be visible on studies performed without intravenous contrast.
The cervix is grasped with two tenacula allergy help best buy for aristocort, and the superficial portion of the lower part of the cardinal ligament is clamped on each side. The bladder is pushed farther inferiorly, with use of the established infrafascial plane within the pubovesical cervical fascia. Note that the vagina is behind and the bladder and ureters are in front of the plane. The position of the ureter must be definitely identified so as not to ligate it during this phase of peritoneal closure. A Zeppelin clamp has been placed on the left cardinal ligament close to the cervix (view from head looking toward feet). The top of the vagina is neatly separated from the bladder and has been sutured closed. The upper margin (cuff) of the vagina is reefed with a running or running lock stitch. In this picture, the suspension has been completed on the left side, and the right side has been sutured but not yet tied into place. Finally, the cut edges of the perineum are approximated by a running suture of 3-0 Vicryl. Subtotal Hysterectomy this procedure is not frequently done, although during the 1940s, 1950s, and even early 1960s, its performance was commonplace. The advantages of the operation are principally speed and a diminished risk of ureteral injury because the cardinal ligaments are not taken down. When the corpus is severed and removed from the field, operative exposure is always positively affected. The descending or cervical branch of the uterine artery is left intact if possible. If this branch is clamped with the larger ascending branch, no difficulty relative to vascular supply to the cervix is encountered because anastomotic branches of the vaginal artery provide ample collateral circulation. Typically, the uterosacral and cardinal ligaments are intact; therefore no suspension is required. On completion of cervical closure, the wound is irrigated to check for bleeding points. I recommend, before the top of the cervical stump is sutured, that the surgeon cut a thin disc from the exposed cervix at the point of separation from the body of the uterus to ensure that no functioning endometrium remains. The intra-abdominal portion of the cervix is closed by a row of interrupted simple or figure-of-8 sutures. In this instance, the utero-ovarian ligament and the oviduct are triply clamped close to the uterine fundus. The incision is made with scissors or knife between the clamp closest to the uterus and the second clamp. Transfixing suture ligatures of 0 Vicryl are placed behind the third (most distant from the uterus) and second clamps. On the left side, three clamps have been placed across the tube and utero-ovarian ligament. Although it bears an ingrained designation as minimally invasive, it clearly is invasive and falls into the category for a major operation. Nevertheless the laparoscopic route and technique have certain advantages and disadvantages. The natural postoperative course or pathway will be one of expected daily improvement. Limitation of angles to manipulate tissues, especially when adhesions are encountered 2. User difficulty in suturing tissues and limitations to needle size, thus resulting in a dependence on "crutches" for hemostasis. Injury risk peculiar to the laparoscopic technique above and beyond the actual operation; principally, the necessity of placing a trocar device into the abdominal cavity However when all aspects of route, advantages, and disadvantages are put aside, the operation of hysterectomy by laparotomy versus laparoscopy is in fact or at least should be more or less identical in technique. The peritoneum that reflected off the dome of the urinary bladder onto the anterior surface of the uterus is dissected from the uterus. Next the posterior sheath of the broad ligament is opened, and a decision is required whether to retain or remove the ovaries. The bladder at this juncture may require further dissection to free it from the anterior wall of the vagina.
The external iliac vein allergy testing for dogs cost cheap aristocort 4mg visa, hypogastric artery and vein, ureter, and ovarian vessels must be identified and secured from injury during adhesiolysis. The latter technique helps the clinician to identify the plane of attachment of the adhesion to a visceral structure and in turn permits the least bloody and least traumatic separation. Adhesions are obviously always best dissected from superficial (first cut) to deep (last cut). The technique used by me for adhesions that are layered consists of making a small, careful nick at the edge of the adhesion, insinuating a fine dissection scissors into the adhesion, and alternately spreading and closing the scissors blade to expose any structure within the adhesion before cutting it. In this manner, a plane of safe dissection is established, allowing the adhesions to be transected sharply. Similarly, one can use a Touhy needle (18 or 22 gauge) to inject saline into the adhesion to facilitate separation. It is curious that the inflammatory response does not necessarily coincide with the severity of endometriosis. Endometriosis surgery is performed after attempts at medical therapy have failed to resolve symptoms and eliminate visible lesions. The radical treatment strategy is removal of the reproductive organs by means of hysterectomy, as illustrated in Chapter 12. A rather confusing term used indiscriminately is "definitive treatment at surgery. Surgical removal of the endometriosis with preservation of the uterus and adnexa is accomplished by sharp excision or laser surgery. Vaporization of implants is performed at a setting of 5 to 10 W at 100 to 300 pulses/sec and 0. Note the extensive inflammatory reaction in the peritoneum surrounding the overt endometrial implants. As these implants are ablated, brownish (hemosiderin) fluid exits from the lesions. Several biopsy-proven vesicular endometrial implants on the fimbriated portion of the oviduct, which is adhesed to the ovary. The water creates a heat sink to protect the underlying muscularis and mucosa of the intestine. Scar formation resulting from the endometriosis distorts the uterus and the round ligaments, which appear to be inserted into the bladder. The colon is held in preparation for ablation (in this case) or excision of the endometriosis. The bladder and the uterus are copiously irrigated on completion of the destruction of all endometriotic implants. Injection of sterile water beneath the implants will create a plane of dissection and a heat sink. The left ovary not only has surface implants but also is enlarged, suggesting the presence of an endometrial cyst. Schema for a secondpuncture laser probe and the laparoscopic technique for treating endometriosis. In this case, single-puncture delivery integrates the operating tool within a single instrument that is also used to provide light and an optical view of the operative field. Note the relative size of the laser channel (left) compared with the optic (right). The uterus and sigmoid were densely adhesed to the cul-de-sac (these have been dissected free). Although most tubal ectopic pregnancies are managed laparoscopically, certain circumstances may require laparotomy. These include large tubal pregnancies, rupture with substantial hemorrhage and hypovolemia, and cornual pregnancies. The open procedure for treating a leaking or unruptured tubal pregnancy is identical to the laparoscopic procedure. Discount aristocort line. Dry Cough- Doctor Live Oct 18 Part 1.
|