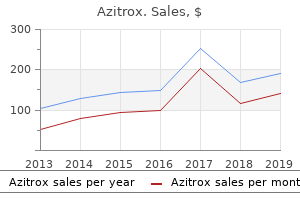
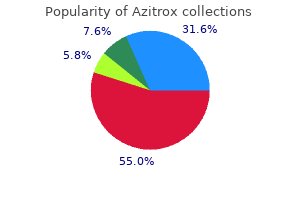
Azitrox"Buy generic azitrox on-line, infection years after knee replacement". By: X. Hamil, M.B. B.CH., M.B.B.Ch., Ph.D. Program Director, University of New Mexico School of Medicine If you have experienced a rapid change in air pressure antibiotics vs antibodies order generic azitrox from india, you probably have noticed your ears "popping" as the air pressure is equalized and the tympanic membrane snaps back into place. The auditory ossicles (os -si-kulz) are three tiny bones that articulate to form a lever system from the tympanic membrane, across the tympanic cavity, to the internal ear. The vibrations of the tympanic membrane cause corresponding movements of the ossicles, which result in the stapes vibrating in the oval window. In this way, vibrations of the tympanic membrane are transmitted to the fluid-filled internal ear. Due to the size difference between the larger tympanic membrane and the smaller oval window, vibrations are amplified by the ossicles. It consists of two series of connecting tubes and chambers, one within the other: an external bony labyrinth (lab i-rinth) and an internal membranous labyrinth. The space between the bony and membranous labyrinths is filled with perilymph, whereas the membranous labyrinth contains endolymph. The internal ear has three major parts: the cochlea, vestibule, and semicircular canals. The scala vestibuli continues into the vestibule, which houses the membrane-covered oval window. The scala tympani extends toward the vestibule, ending at the membrane-covered round window. Perilymph fills the space between the membranous labyrinth and the bony labyrinth. Note that the ampullae of the semicircular canals, utricle, saccule, and cochlear duct are portions of the membranous labyrinth. The cochlear duct, which is part of the membranous labyrinth, extends nearly to the apex of the cochlea (see figure 9. The basilar membrane contains about 20,000 cross fibers that gradually increase in length from the base to the apex of the cochlea. The attachment of the basilar membrane to the bony center of the cochlea allows it to vibrate like the reeds of a harmonica when activated by vibrations generated by sound. The spiral organ (organ of Corti), which contains the sensory receptors for sound stimuli, supported by the basilar membrane within the cochlear duct. Physiology of Hearing the human ear is able to detect sound waves with frequencies ranging from near 20 to 20,000 Hertz (Hz; vibrations per second), but hearing is most acute between 2,000 and 3,000 Hz. Then, the cochlear hair cells form nerve impulses that are transmitted to the hearing areas of the cerebrum for interpretation as sound sensations. Sound waves enter the external acoustic meatus and strike the tympanic membrane, causing it to vibrate in and out at the same frequency and comparable intensity to the sound waves. Loud sounds cause a greater displacement of the tympanic membrane than do soft sounds. Vibration of the tympanic membrane causes movement of the auditory ossicles, resulting in the in-and-out vibration of the stapes in the oval window. The vibration of the stapes causes a corresponding oscillatory (back-and-forth) movement of the perilymph in the scala vestibuli and scala tympani and a corresponding movement of the membrane over the round window. This movement of the perilymph causes vibrations in the vestibular and basilar membranes. The vibration of the basilar membrane causes the stereocilia of the cochlear hair cells to contact the tectorial membrane, which stimulates the formation of nerve impulses by the cochlear hair cells. Nerve impulses formed by the cochlear hair cells are carried by the cochlear branch of the vestibulocochlear nerve to the hearing areas of the temporal lobes of the cerebrum, where the sensation is interpreted. Pinilla L antibiotic basics for clinicians cheap 250 mg azitrox amex, Aguilar E, Dieguez C, et al: Kisspeptins and reproduction: physiological roles and regulatory mechanisms. Often, endometriosis occludes the fallopian tubes, either at the fimbriated ends or elsewhere along their extent. Another common cause of female infertility is salpingitis, that is, inflammation of the fallopian tubes; this inflammation causes fibrosis in the tubes, thereby occluding them. In the past, such inflammation occurred mainly as a result of gonococcal infection. However, with modern therapy, salpingitis is becoming a less prevalent cause of female infertility. Still another cause of infertility is secretion of abnormal mucus by the uterine cervix. Ordinarily, at the time of ovulation, the hormonal environment of estrogen causes the secretion of mucus with special characteristics that allow rapid mobility of sperm into the uterus and actually guide the sperm up along mucous "threads. If the ovum becomes fertilized, a new sequence of events called gestation or pregnancy takes place, and the fertilized ovum eventually develops into a full-term fetus. The purpose of this chapter is to discuss the early stages of ovum development after fertilization and then to discuss the physiology of pregnancy. In Chapter 84, some special aspects of fetal and early childhood physiology are discussed. After the male ejaculates semen into the vagina during intercourse, a few sperm are transported within 5 to 10 minutes upward from the vagina and through the uterus and fallopian tubes to the ampullae of the fallopian tubes near the ovarian ends of the tubes. This transport of the sperm is aided by contractions of the uterus and fallopian tubes stimulated by prostaglandins in the male seminal fluid and also by oxytocin released from the posterior pituitary gland of the female during her orgasm. Of the almost half a billion sperm deposited in the vagina, a few thousand succeed in reaching each ampulla. Fertilization of the ovum normally takes place in the ampulla of one of the fallopian tubes soon after both the sperm and the ovum enter the ampulla. Before a sperm can enter the ovum, however, it must first penetrate the multiple layers of granulosa cells attached to the outside of the ovum (the corona radiata) and then bind to and penetrate the zona pellucida surrounding the ovum. Once a sperm has entered the ovum (which is still in the secondary oocyte stage of development), the oocyte divides again to form the mature ovum plus a second polar body that is expelled. The mature ovum still carries in its nucleus (now called the female pronucleus) 23 chromosomes. Shortly before it is released from the ovarian follicle, its nucleus divides by meiosis and a first polar body is expelled from the nucleus of the oocyte. In this process, each of the 23 pairs of chromosomes loses one of its partners, which becomes incorporated in a polar body that is expelled. It is at this time that the ovum, which is still in the secondary oocyte stage, is ovulated into the abdominal cavity. Then, almost immediately, it enters the fimbriated end of one of the fallopian tubes. When ovulation occurs, the ovum, along with a hundred or more attached granulosa cells that constitute the corona radiata, is expelled directly into the peritoneal cavity and must then enter one of the fallopian tubes (also called uterine tubes) to reach the cavity of the uterus. The inner surfaces of the fimbriated tentacles are lined with ciliated epithelium, and the cilia are activated by estrogen from the ovaries, which causes the cilia to beat toward the opening, or ostium, of the involved fallopian tube. Although one might suspect that many ova fail to enter the fallopian tubes, conception studies suggest that up to 98 percent of ova succeed in this task. E, Reorganization of a full complement of chromosomes and beginning division of the ovum. B,Theaction of trophoblast cells in implantation of the blastocyst in the uterine endometrium. This transport is effected mainly by a feeble fluid current in the tube resulting from epithelial secretion plus action of the ciliated epithelium that lines the tube; the cilia always beat toward the uterus. The fallopian tubes are lined with a rugged cryptoid surface that impedes passage of the ovum despite the fluid current. Also, the isthmus of the fallopian tube (the last 2 centimeters before the tube enters the uterus) remains spastically contracted for about the first 3 days after ovulation. After this time, the rapidly increasing progesterone secreted by the ovarian corpus luteum first promotes increasing progesterone receptors on the fallopian tube smooth muscle cells; then the progesterone activates the receptors, exerting a tubular relaxing effect that allows entry of the ovum into the uterus. This delayed transport of the fertilized ovum through the fallopian tube allows several stages of cell division to 1056 occur before the dividing ovum-now called a blastocyst, with about 100 cells-enters the uterus. During this time, the fallopian tube secretory cells produce large quantities of secretions used for the nutrition of the developing blastocyst. Order genuine azitrox on line. Grapefruit Seed Extract Benefits: It's a Candida Killer & More!.
Likewise infection leg azitrox 250 mg amex, administration of large doses of cortisol causes significant atrophy of lymphoid tissue throughout the body, which in turn decreases the output of T cells and antibodies from the lymphoid tissue. As a result, the level of immunity for almost all foreign invaders of the body is decreased. This decrease occasionally can lead to fulminating infection and death from diseases that would otherwise not be lethal, such as fulminating tuberculosis in a person whose disease had previously been arrested. However, this ability of cortisol and other glucocorticoids to suppress immunity makes them useful drugs in preventing immunological rejection of transplanted hearts, kidneys, and other tissues. Cortisol increases the production of red blood cells by mechanisms that are unclear. When excess cortisol is secreted by the adrenal glands, polycythemia often results, and conversely, when the adrenal glands secrete no cortisol, anemia often results. Cellular Mechanism of Cortisol Action Cortisol, like other steroid hormones, exerts its effects by first interacting with intracellular receptors in target cells. Because cortisol is lipid soluble, it can easily diffuse through the cell membrane. Other proteins in the cell, called transcription factors, are also necessary for the hormone-receptor complex to interact appropriately with the glucocorticoid response elements. Thus, most of the metabolic effects of cortisol are not immediate but require 45 to 60 minutes for proteins to be synthesized, and up to several hours or days to fully develop. Recent evidence suggests that glucocorticoids, especially at high concentrations, may also have some rapid nongenomic effects on cell membrane ion transport that may contribute to their therapeutic benefits. This hormone, also called corticotropin or adrenocorticotropin, also enhances the production of adrenal androgens. This nucleus in turn receives many nervous connections from the limbic system and lower brain stem. Within minutes the entire control sequence leads to large quantities of cortisol in the blood. This increase is believed to result from increased activity in the limbic system, especially in the region of the amygdala and hippocampus, both of which then transmit signals to the posterior medial hypothalamus. The key to this control is the excitation of the hypothalamus by different types of stress. Stress stimuli activate the entire system to cause rapid release of cortisol, and the cortisol in turn initiates a series of metabolic effects directed toward relieving the damaging nature of the stressful state. Direct feedback of the cortisol to both the hypothalamus and the anterior pituitary gland also occurs to decrease the concentration of cortisol in the plasma at times when the body is not experiencing stress. This effect results from a 24-hour cyclical alteration in the signals from the hypothalamus that cause cortisol secretion. Therefore, measurements of blood cortisol levels are meaningful only when expressed in terms of the time in the cycle at which the measurements are made. The effect is much greater in people who have genetically dark skins than in light-skinned people. In some animals, an intermediate "lobe" of the pituitary gland, called the pars intermedia, is highly developed, lying between the anterior and posterior pituitary lobes. Furthermore, this secretion is independently controlled by the hypothalamus in response to the amount of light to which the animal is exposed or in response to other environmental factors. For instance, some arctic animals develop darkened fur in the summer and yet have entirely white fur in the winter. Adrenal Androgens Several moderately active male sex hormones called adrenal androgens (the most important of which is dehy droepiandrosterone) are continually secreted by the adrenal cortex, especially during fetal life, as discussed in Chapter 84. Also, progesterone and estrogens, which are female sex hormones, are secreted in minute quantities. It is possible that part of the early development of the male sex organs results from childhood secretion of adrenal androgens. The adrenal androgens also exert mild effects in the female, not only before puberty but also throughout life. Much of the growth of the pubic and axillary hair in the female results from the action of these hormones. Exner D can antibiotics for uti delay your period buy 500 mg azitrox fast delivery, Dries D, Domanski M, et al: Lesser response to angiotensin-converting-enzyme inhibitor therapy in black as compared with white patients with left ventricular dysfunction. Dries D, Exner D, Gersh B, et al: Racial differences in the outcome of left ventricular dysfunction. Dries D, Strong M, Cooper R, et al: Efficacy of angiotensin-converting enzyme inhibition in reducing progression from asymptomatic left ventricular dysfunction to symptomatic heart failure in black and white patients. Yancy C, Fowler M, Colucci W, et al: Race and the response to adrenergic blockade with carvedilol in patients with chronic heart failure. Eichhorn E, Domanski M, Krause-Steinrauf H, et al: A trial of the beta-blocker bucindolol in patients with advanced chronic heart failure. Although pharmacologic approaches have been responsible for significant reductions in heart failure mortality, attempts to make further gains by adding additional agents have largely been unsuccessful. Additionally, currently used pharmacologic therapies slow the progress of the remodeling but do not address the underlying cause, namely critical loss of contractile myocardium in the infarcted area. Although heart transplantation is an option when pharmacologic therapies fail, it is severely limited because the need exceeds organ availability 10-fold, and the long-term effects of rejection and side effects of immunosuppression have limited its durability (median survival post transplant is 9 years). Several new biologic therapies and strategies for the treatment of heart failure have emerged in recent years, which will be reviewed in this chapter. Two main approaches will be reviewed here, including cardiac cell therapy and gene therapy, which hold great promise for changing our current approach to heart failure treatment. First proposed in the 1990s, cell replacement therapy was an attempt by investigators to address the limited availability of donor organs for cardiac transplantation. For lack of a better alternative, the first cell type tested was skeletal muscle cells. Most studies have focused on the first two cell types because of a report in 2001 in which circulating cells were harvested and reinjected into the heart after treatment with cytokines commonly used to mobilize hematopoietic stem cells. These studies did not demonstrate any significant conversion of c-kit expressing bone marrow cell conversion into cardiomyocytes or any significant capacity of these cells to restore heart function. Schematic diagram Pluripotent stem cells Pluripotent stem cells Programmed directed-differentiation Programmed directed-differentiation outlining the sources of adult cells types that have been used for cardiac cell therapy. Regardless, several of these circulating cell types have made their way into the clinics and are currently being tested for clinical efficacy. Bone marrow, the presumed source of the c-kit+ and other circulating progenitor cells, has been used extensively in preclinical and clinical trials. Although the exact regenerative capability of each of these cell types is strongly debated, positive preclinical studies have resulted in numerous phase I clinical trials. However, to date, there is no direct evidence that any bone marrow cell can differentiate into a mature cardiomyocyte (without genetic reprogramming), so any regenerative effects are most likely indirect. Several endogenous or resident cardiac stem cell/ progenitors have now been described. These cardiac c-kit cells could be isolated and transplanted into recipient animals, reconstituting the infarcted ventricular wall and reducing infarct size. They have the capacity to differentiate into cells of all three germ lines, including cardiac myocytes. Somatic cells such as skin fibroblasts can be reprogrammed to a pluripotent state with a cocktail of reprogramming factors. Finally, a cardiac progenitor cell has been reported to exist in cardiospheres, although its identity remains unknown. These cells retain the potential to differentiate into any cell type if given the appropriate growth factors. These cells can grow and divide within the recipient heart, as well as form gap junctions and become electrically coupled to the host myocardium. In postinfarct models, not only have these cells proven to improve function but have also demonstrated reduced rates of ventricular arrhythmia either spontaneously or with attempted induction through electrical stimulation. In 1996, the sheep, Dolly, was cloned by a method of transferring the nucleus from a somatic cell (in her case the mammary gland) to an unfertilized egg,35 thus proving in the correct setting a cell can be converted to any other cell type.
|