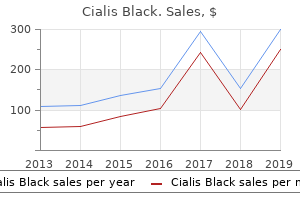
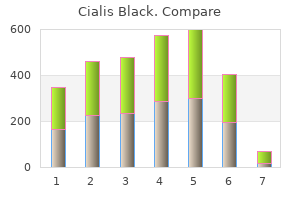
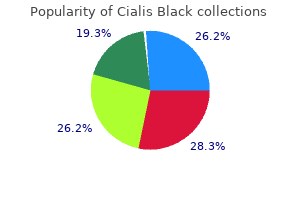
Cialis Black"800 mg cialis black otc, erectile dysfunction over the counter medications". By: K. Kaelin, M.A.S., M.D. Co-Director, Johns Hopkins University School of Medicine In cases of massive blood loss or suspicion of coexisting abruption erectile dysfunction pills amazon discount cialis black 800mg free shipping, fibrinogen level, Kleihauer test, and prothrombin time should be checked. Cell salvage may be considered, especially in women who refuse donor blood [9,10]. Incision Cesarean section is usually performed through a transverse or Pfannenstiel skin incision. Careful ultrasound mapping of the placental site before surgery may assist the surgeon in planning the direction of uterine incision [3,4]. In the case of anterior placenta, a transverse incision is made in the lower uterine segment. The placenta will be met underneath the uterine incision; the baby may be delivered by the obstetrician passing a hand around the margins of the placenta. If the placenta is cut, the baby should be delivered immediately, and immediate cord clamping is essential to prevent fetal exsanguination. If the placenta is in anterolateral location, a low vertical incision can be made in the lower uterine segment on the opposite side from the placenta. If the placenta wraps around the cervix from anterior to posterior lower uterine segment, a transverse or vertical incision may be possible above it, although it may lead to extension into upper uterine segment [11,12]. Management timing of delivery the timing of delivery depends on maternal and fetal conditions. Elective delivery by cesarean section is recommended at or after 38 weeks of gestation for asymptomatic women with major placenta praevia [3]. However, about 40% of women with major placenta praevia deliver before 38 weeks of gestation. Emergency delivery by cesarean section is indicated in women with vaginal bleeding with fetal heart rate abnormalities, life-threatening maternal hemorrhage, and onset of labor with major praevia [4]. If there is recurrent bleeding, particularly after 34 weeks of gestation, delivery may be considered. After a diagnosis of Gynecologic and Obstetric Surgery: Challenges and Management Options, First Edition. It is important to always anticipate massive obstetric hemorrhage in a woman with placenta praevia. The suture is passed through the uterine cavity to emerge at the upper incision margin 3 cm above and approximately 4 cm from the lateral border (because the uterus widens from below upward). The suture is fed through posteriorly and vertically over the fundus to lie anteriorly and vertically compressing the fundus on the right side, in a similar fashion to the left side. The two lengths of the suture are pulled tightly assisted by bimanual compression to minimize trauma, and a secure knot is placed. Parallel vertical compression sutures [15] B-Lynch compression suture [14] the patient is placed in Lloyd-Davies position for access to the vagina to assess the control of bleeding. A round-bodied needle Cesarean section with a Pfannenstiel incision is performed in the usual way. After the placenta is removed, the bladder is reflected downward so as to adequately expose the underlying lower uterine segment. The exact entry and exit sites of the needle can be positioned in the lower segment as needed near the site of active bleeding so as to achieve effective compression of the bleeding vessels. Hemostasis was achieved by hemostatic square sutures placed in the placental bed and an intrauterine tamponade balloon. Placental edge to internal os distance in the late third trimester and mode of delivery in placenta praevia. The anaesthetic management of caesarean section for placenta praevia: a questionnaire survey. Ceasarean section for placenta praevia: a retrospective study of anaesthetic management. A survey of the anaesthetic management of patients presenting for caesarean section with high risk obstetric conditions. Five-year study assessing the feasibility and safety of autologous blood transfusion in pregnant Japanese women.
Laparoscopicassisted vaginal hysterectomy for patients with extensive pelvic adhesions: a strategy to minimise conversion to laparotomy erectile dysfunction tucson generic 800 mg cialis black free shipping. Benefits and harms of adhesion barriers for abdominal surgery: a systematic review and meta-analysis. Peritoneal full conditioning reduces postoperative adhesions and pain: a randomised controlled trial in deep endometriosis surgery. She developed an incisional hernia, which was repaired laparoscopically 7 years ago. It is not uncommon that the operating surgeon will have to see, assess, and subsequently operate on a variety of patients that have had previous abdominal surgery. The incidence of incisional hernia after major laparotomy is up to 20% but at least 10% of wounds will have a defect that is symptomatic [1]. Most present within the first year and the rates are doubled in the presence of infection at the index operation. The modern management of incisional hernia is very varied and many techniques and meshes have been popularized over the last 20 years to try to surgically ameliorate this common problem. High rates of recurrence with suture repair (up to 54%) [3] have promoted the routine use of mesh to reduce recurrence rates [4]. Laparoscopic repair may have benefits in primary ventral or incisional hernia repair and the technique has been shown to be safe when compared with open surgery [5,6]. It is important to have a basic understanding of the different approaches to incisional hernia repair and the different meshes that are used, to enable a safe approach to managing patients who require a subsequent laparotomy. The large number of defects created, subsequent repairs, routine use of mesh, and vogue for laparoscopic surgery makes this a challenge for the operating surgeon. As patients live longer and more repairs are performed, we conclude this will become an increasingly common challenge. Many patients requiring laparotomy may have had intra-abdominal meshes placed laparoscopically for the treatment of primary ventral hernia. Scars from this procedure may be difficult to see as there is no primary incision. However, these will generate the same issues of concern for the operating surgeon on entry to , and closure of, the abdomen. It is important to look for evidence of this repair, both clinically and in the past surgical history assessment. Most scars will be found laterally toward the mid-axillary line, as a lateral approach to port placement is required to facilitate mesh placement. Similarly, some mesh techniques use a small incision in the skin and the rectus sheath but are used to place large meshes (up to 30 cm) caudally and cephalad undermining the respective layers. They are all treated similarly at repeat laparotomy but knowledge of what might be found and in what layer may help the surgeon, especially if a mesh is unexpectedly encountered. Simple meshes are inert polymers that form a matrix for intense fibrosis to strengthen a repair. They cause a local reaction that changes the nature of the underlying and overlying tissues, and the subsequent fibrosis (characterized by an intense white reaction) reinforces what would otherwise be a weak repair. They are generally used for repairs where the mesh is placed outside the peritoneum because of concerns of mesh enterocutaneous fistulation or adhesive small bowel obstruction. Component meshes were conceived to combat this problem and allow intraperitoneal placement to facilitate repairs where mesh could not be placed outside the peritoneal cavity. These usually comprise one of the simple polymers but have a specialist layer that is hydrophilic in nature and safer in contact with bowel. It is important to remember that these meshes are designed to facilitate regeneration of the peritoneum, with a full covering within 2 weeks. Subsequently, they can be difficult to see if the abdomen is opened away from the hernia site repair. Their use is increasing as they offer a solution to incisional hernia repairs in cases where the risk of infection is very high. Surgical techniques It is not necessary to know the intimate details of all types of repairs but some fundamental knowledge will help the operating gynecologist react to , and manage, patients with a previous mesh insertion. Whether the mesh is placed laparoscopically or via open surgery is largely irrelevant, but all laparoscopic meshes are placed within the abdomen and normally fixed with a combination of sutures and tacking devices. In general, large meshes are used to obtain a greater than 5-cm overlap of the defects to reduce recurrence.
It is crucial to identify the sling prior to cutting or excising it; a transurethral Hegar dilator can help localize the sling accurately impotence examination cialis black 800 mg low cost. A right-angle clamp may be placed between the sling and the periurethral fascia to avoid injury to the urethra. Voiding dysfunction after surgery for stress incontinence: literature review and survey results. Treatment success of retropubic and transobturator mid urethral slings at 24 months. Obstruction following anti-incontinence procedures: diagnosis and treatment with transvaginal urethrolysis. The utility of urodynamics in clinically suspected obstruction after anti-incontinence surgery in women. Tape mobilization for urinary retention after tension-free vaginal tape procedures. Release of tension-free vaginal tape for the treatment of refractory postoperative voiding dysfunction. The efficacy of urethrolysis without re-suspension for iatrogenic urethral obstruction. Minimally invasive synthetic suburethral sling operations for stress urinary incontinence in women. Flexible cystoscopy reveals a portion of the tape eroded into the bladder with an attached calculus. Foreign material extruding into the bladder has also been described following mesh repair of pelvic organ prolapse, and following the use of non-absorbable sutures at colposuspension. Surgery is best done by a urologist or a urogynecologist with experience in reconstructive surgery. Bladder perforation, if intraoperatively recognized, can be managed by re-passage of the trocar and prolonged catheter drainage of the bladder postoperatively (Chapters 35 and 102). Erosion is the postoperative appearance of tape material in the bladder or the urethra. Bladder erosion usually represents an undiscovered intraoperative perforation; urethral erosion, on the other hand, is usually due to migration of foreign material, with presentation typically after a long period [4]. In one series of 14 patients, presentation was with dysuria, hematuria, urge incontinence, urinary frequency, and pelvic pain [5]. Intraoperative detection of a bladder perforation is the standard method of minimizing the risk of erosion. Routine cystoscopy can identify otherwise undetected Various methods for transurethral removal of eroded vesical tape have been described. Eroded foreign material can be elevated, with holmium laser resecting the margins close to the bladder mucosa. Endoscopic resection using operative cystoscope and hysteroscopic scissors, laparoscopic endoshears and lighted nasal speculum has also been described [2,8]. Endoscopic techniques are minimally invasive and have low morbidity; however, endoscopic resection is more limited than open techniques in the amount of material accessible for removal, and persistent or recurrent tape exposure is more common. Techniques to maximize the length of excised tape include traction on the extruding tape utilizing hemostatic clip or other clamps. Suprapubic telescopy using a 5-mm laparoscopic trocar placed into the bladder dome allows for use of laparoscopic scissors or a grasper while the opposite instrument can be placed through the cystoscopic sheath to allow excision of the exposed tape. Transurethral cystolitholapaxy, or pneumatic or laser lithotripsy can be utilized if significant encrustation or calculus formation has occurred on the exposed tape. With local anesthetic and epinephrine as hemostatic agents, a midline or inverted-U vaginal incision is made suburethrally to the bladder base, exposing the tape to be dissected free. Alternate techniques have used a combination of an operating cystoscope and 5-mm suprapubic ports [11]. Open surgery Laparoscopic management Laparoscopic transvesical resection of eroded bladder tape has been described by several authors. One technique involves filling the bladder with carbon dioxide and placing three 5-mm ports in the lower abdomen directly into the bladder, excising the tape extruding from the bladder muscle layer completely, and removing it with any Erosions at the bladder dome are more easily exposed via an open approach. A low Pfannenstiel incision allows retropubic extraperitoneal access to enable cystotomy at the dome revealing the exposed mesh [12].
Unsalvageable bowel may include fibrotic strictures and severely diseased bowel causing abscesses or fistulae erectile dysfunction treatment mayo clinic cialis black 800 mg lowest price. When encountered incidentally at laparoscopy, it is helpful for future management to "run the small bowel," documenting the number of sites involved; however, resection is often best avoided in this setting. Bowel adhesions and strictures Bowel obstruction secondary to adhesions usually presents to general surgeons with symptoms of acute bowel obstruction: cramping abdominal pain, distension, vomiting, and failure to open bowels. However, most adhesions seen at laparotomy or laparoscopy by gynecologists are usually long-standing. Adhesiolysis risks serosal tears and enterotomies, and may cause prolonged ileus postoperatively. Strictures of the small bowel may similarly present with acute bowel obstruction, but sometimes the obstruction may be of gradual onset. Therefore, loops of dilated small bowel may be found as an incidental finding, with collapsed loops seen distal to the obstruction. Since bypass of small bowel segments may cause bacterial overgrowth in excluded small intestinal loops, resection is performed where possible; however, bypass may be necessary in the palliative setting where it may not be possible to mobilize small bowel away from a tumor in the pelvis, for example. A third option is to perform a diverting stoma, which avoids anastomosis of thickened edematous bowel. Bowel tumors Colorectal malignancy is often asymptomatic, particularly when occurring in the proximal colon. Tumors may be noted incidentally if they have breached the serosal surface of the bowel, or if there is evidence of bowel obstruction. In addition, colorectal cancer may metastasize to the ovary(s), a condition known as Krukenberg tumor. Therefore bowel cancer is not infrequently seen in patients with malignancy of the gynecologic tract. The diagnosis is usually confirmed by colonoscopic biopsy (unless there are obvious peritoneal nodules which can be sampled at the initial laparoscopy) and imaging undertaken for staging purposes. Further management is then decided by the multidisciplinary team, and may include options such as bowel resection with or without stoma, colonic stenting, and the possibility of neoadjuvant therapy. In the case of umbilical hernias, entry into the abdomen by entering the hernia sac is often straightforward, and careful closure of the port site will often suffice to coincidentally repair the hernia. Pneumoperitoneum may make inguinal hernias evident externally, and at laparoscopy bowel may be noted to enter the inguinal canal. Inguinal hernias and larger incisional hernias require a mesh repair; to reduce the risks of infection, hernia repair is best done as a stand-alone procedure where possible. Incisional hernias arising from scars in the lower abdomen can be challenging to repair laparoscopically via a transabdominal approach. Since the bladder is an extraperitoneal organ, bladder expansion will tend to strip the mesh off the undersurface of the abdominal wall. For this reason, some surgeons repair this hernia by creating an extraperitoneal pocket for the inferior edge of the mesh. Chapter 33: Unexpected Pathology: Abnormal Appearance of Bowel 99 Immediate definitive operative management of the diverticular disease is usually not indicated, but the opportunity afforded by laparoscopy can help in two ways. Firstly, collections of pus can be drained, and laparoscopic lavage may also help to control infection. Secondly, laparoscopy can allow a general surgeon an opportunity for planning future operative intervention in patients less acutely unwell. For example, he or she may want to ascertain the extent of the diverticular disease and the potential involvement of adjacent and retroperitoneal structures. In cases at high risk of bowel pathology, having a general or colorectal surgeon on standby is prudent. If unexpected bowel pathology is identified and a surgeon is not available for an intraoperative opinion, a video recording of systematic examination of the bowel can help later review by the surgeon. Close team-working between general surgeons and gynecologists will ensure the best outcomes for women with intestinal problems presenting to gynecologic surgeons. 800mg cialis black free shipping. Permanently Cure Erectile Dysfunction | Explained in English | Arogyam.
|