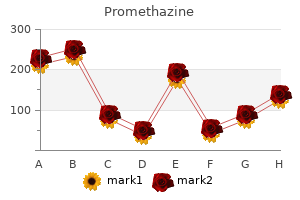
Promethazine"Order promethazine 25 mg free shipping, allergy medicine nasal spray". By: A. Ford, M.A., M.D. Assistant Professor, Columbia University Roy and Diana Vagelos College of Physicians and Surgeons The most effective preventive measure is meticulous preservation of the periosteum and other soft tissues overlying the bony surfaces adjacent to the intended fusion surface allergy shots yahoo answers order promethazine on line amex. A new occipitocervical fusion construct in pediatric patients with occipitocervical instability. Inside-outside technique for posterior occipitocervical spine instrumentation and stabilization: preliminary results. Spinal cord injury without radiographic abnormalities in children, 2 decades later. Atlanto-axial rotatory fixation Part I: biomechanics of normal rotation at the alanto-axial joint in children. Hypermobility of the cervical spine in children: a pitfall in the diagnosis of cervical dislocation. Paraplegia in hyperextension cervical injuries with normal radiographic appearances. A special slender perforated stem (between the arrows) has been adapted for sublaminar wiring onto delicate laminae. Problems with Fusion Extension Unintentional inclusion of adjacent "bystander" vertebrae into the fusion mass sometimes occurs in children. Children have a greater capacity than adults to form exuberant callus whenever the periosteum is breached and the neck is effectively immobilized. Migration of bone grafts seems to be less important because as long as the periosteum is intact, stray grafts do not promote bystander fusion. Final nut tightening onto the vertical axis plate is accomplished with a socket wrench (black arrow), and a screw driver (white arrow) is inserted into the hollow hex of the inside-outside screw stem to provide counter-torque. Note the slender perforated lower stem for sublaminar cables (already fastened with crimpers). The motor disorders of cerebral palsy are often accompanied by disturbances of sensation, cognition, communication, perception and/or behavioral and/or by a seizure disorder. However, there is great disparity among practitioners regarding the use of these terms, such that a given patient may be classified differently by different clinicians. In 2000, the Surveillance for Cerebral Palsy in Europe group adopted a standardized system for database and registry purposes that is used throughout Europe and Australia. Dissecting out and treating, as possible, the various abnormalities will have the biggest impact on future motor outcome. Evaluation begins with a detailed history and physical and neurological examination, including careful documentation of prenatal, perinatal, and neonatal events and risk factors, developmental milestones, family history, general medical history, and a detailed survey to look for associated impairments. An atypical history, clinical features, or imaging findings should trigger further evaluation, especially if there is any history of developmental regression or loss of skills. Conversely, nonverbal learning disorders may be missed in a child with superior verbal skills. Children with severe mobility impairments tend to be less healthy and spend more time in bed and more days in the hospital, are more likely to be malnourished, and are often taking more medications than their nondisabled peers. The prevalence of significant pathology (increased detrusor muscle contraction, reduced detrusor muscle compliance, reduced bladder capacity, inability to relax the external urethral sphincter, and high postvoid residuals) may be as high as 97%29-33 and can increase the risk for progressive decline in upper urinary tract function and renal disease. The therapist has a pivotal role as a teacher to help patients master new motor skills and teach parents (and older patients) exercises (stretching, strengthening, balance) and adaptive techniques (assistive technology for activities of daily living, access to computers or communication devices) that they can integrate into their daily life. Detailed neuropsychological testing should be performed before a child starts school. Accurate assessment is difficult if not impossible in many children because of their multiple other impairments. May be beneficial in reducing the spastic component when spasticity far exceeds the dystonia and the patient has good upper extremity function in one or both hands. Strengthening exercises to reverse disuse atrophy may improve gait and do not worsen the spasticity. Management of Hypertonia and Spasticity in Children with Cerebral Palsy Hypertonia is defined as abnormally increased resistance to externally imposed movement about a joint. The Task Force on Childhood Motor Disorders recently developed a consensus definition of spasticity as "hypertonia in which one or both of the following signs are present: (1) resistance to externally imposed movement increases with increasing speed of stretch and varies with the direction of joint movement, and/or (2) resistance to externally imposed movement rises rapidly above a threshold speed or joint angle.
The pectoralis major is innervated by the medial and lateral pectoral nerves, each a branch of the medial and lateral cords, respectively allergy shots kelowna promethazine 25mg discount. The medial pectoral nerve innervates the sternal head of the pectoralis major, and the lateral pectoral nerve innervates the clavicular head. The Bernard-Horner sign is highly indicative of but not conclusive for avulsion of C8 and T1. False negative (absence of the sign with severe injury) is more common than false positive. The finding may not be present during the first 48 hours after injury and can also fade over time. Starting distally and progressing toward the lesion site, tingling is perceived as soon as the frontal tip of the down-growing highly sensitive but not yet myelinated fibers is met. Serial examination demonstrating distal shift of this point determines the presence and rate of growth of regenerating axons. However, an advancing Tinel sign does not indicate the number or quality of regenerating axons and does not guarantee functional outcome. They can help determine the nerves injured, the location of the injury, and the presence of regeneration. Electrodiagnostic studies are an important adjunct to a thorough history, physical examination, and imaging studies, not a substitute for them. Reduced recruitment of motor units occurs with axonal injury; however, the presence of motor units under voluntary control indicates a nerve in continuity and a good prognosis. Reinnervation potentials (nascent motor units, polyphasic action potentials) appear in a muscle several weeks in advance of clinical evidence of recovery. An injury proximal to the dorsal root ganglion will spare the sensory axons because the cell body remains in continuity with the axons. Imaging of the spine and chest can provide valuable insight on the nature and extent of the injury. A spinal transverse process fracture can be associated with nerve root injury or avulsion. An elevated hemidiaphragm suggests a phrenic nerve issue and probably C3, C4, and C5 spinal nerve injury. Preoperative diagnosis of a preganglionic or root avulsion injury indicates the need for early surgery and use of nerve transfers. One standard for the diagnosis of root avulsion is laminectomy with direct visualization of the roots. This can be modified to a minimally invasive procedure using an endoscope63; however, it has not become a commonly used technique. In the acute situation, an intradural blood clot can prevent filling of a pseudomeningocele. Overall, 70% had supraclavicular lesions; of these, 70% had at least one root avulsed. At least 70% of patients with a root avulsion have avulsions of the lower roots (C7, C8, or T1). Finally, of patients with lower root avulsion, nearly 70% will experience persistent pain. Early surgery allows identification of the nerve ends and frequently a direct end-to-end repair of Sunderland V injuries. When there is evidence of a Sunderland V (rupture) injury as a result of a stretch mechanism at the site of transection, the nerve ends often need to be resected back to a more healthy region. Demarcation of the injury can be difficult to appreciate acutely, and 2 to 3 weeks is generally required for the injury to declare itself. This delay allows more effective trimming of the stumps to healthy tissue and results in better outcomes. For gunshot wounds, a low-velocity projectile is often associated with Sunderland grade I injuries, whereas high-velocity projectiles cause more soft tissue disruption and higher grade Sunderland injury. Animal research has confirmed the clinical suspicion that delay in surgical repair will degrade the eventual outcome, so a balance must be maintained between waiting to see whether spontaneous regeneration will occur versus opting for surgical intervention.
In specific cases, intermediate osteotomies can be performed to mobilize some or all of the malar bones and the inferior orbital rim to a variable degree allergy testing gainesville fl buy cheap promethazine 25 mg on-line. Its two major drawbacks are the magnitude of the operation and the risk for infection (meningitis or osteomyelitis) from the communication between the anterior cranial base and the nasal cavities. It is possible to close this communication with the use of bone grafts and periosteal flaps, but the higher risk for infection remains. The distraction concept using the Ilizarov principle of bony elongation (osteotomy and slow widening of the gap, with progressive creation of new bone and loosening of soft tissues) has been applied to the face. In 1995 we devised an inner distractor for the upper maxilla, which was especially useful in children in whom stable interdental fixation is difficult to achieve. In 2000, in collaboration with Eric Arnaud we devised a frontofacial monobloc distraction system with four distractors, two for the maxilla and two for the forehead, to allow progressive advancement. In this manner, the expanding frontal lobes will gradually fill the space created by the advancement, and the infection rate is very low in our series (4 infections in 73 monobloc advancements with buried inner distractors). The advancement is usually achieved in 2 weeks, a few millimeters a day, and the distractors are removed after 6 to 9 months. Many teams are using the same principle of progressive distraction, but with an external halo-type device fixed on the cranium and pulling anteriorly and wires fixed on the bandeau and maxilla. Indications In infants, the senior authors perform a frontal advancement of the bandeau, up until the age of 5 months. In an older infant, a horizontal tongue-in-groove procedure is the operation of choice. It is now always a distraction procedure, much safer then the classic one-stage advancement. In children, if the forehead has been advanced earlier and is satisfactory, we postpone the facial advancement for as long as possible. The ideal is to wait until eruption of the final dentition, at about 11 or 12 years of age. If the facial retrusion is severe and is creating functional (respiratory and masticatory) or psychological problems, we operate before school age, at about 5 years of age. In unoperated patients or if the forehead still recedes, a monobloc frontofacial advancement is considered in favorable cases, and it is always now done with distraction. If the family prefers to avoid the infectious risks still linked to monobloc advancement, a two-stage operation is performed-frontal advancement first and facial advancement 6 to 9 months later. It is often possible to further improve the appearance of the patient, when growth is almost completed, by frontal contouring, rhinoplasty, genioplasty, orthodontics, and sometimes, orthognathic surgery. Simultaneous Frontal and Facial Advancement In 1971, Tessier described simultaneous advancement of the forehead and face in children with faciocraniosynostosis. Ortiz-Monasterio and colleagues in 1978 proposed performing a monobloc advancement in which the orbits and face are mobilized simultaneously and the upper part of the forehead is adjusted above, as required. The two hemifaces can be moved, the orbits brought in closer together, and the upper maxillae widened. Simultaneous frontofacial advancement is logical because it permits correction of the frontal and facial problems of faciocra- Treatment of Associated Hydrocephalus the association of craniosynostosis and hydrocephalus poses a difficult surgical problem. Treating both problems at the same time produces a dead space between the skull and brain that is not obliterated fast enough, with brain expansion being thwarted by shunting of cerebrospinal fluid. The question is to determine which must be treated first, the craniosynostosis or hydrocephalus. If the hydrocephalus is mild and slowly progressive, the craniosynostosis should be treated first. In this case, a shunt can be used to treat the hydrocephalus, if necessary, after brain reexpansion has been completed. If the hydrocephalus is considerable or rapidly progressive, the shunting should be performed first. A programmable valve may be helpful in avoiding too rapid decompression of the ventricular system. The reduction in size of the ventricles is then monitored by computed tomography, and the craniosynostosis is treated after the size of the ventricles has decreased and is stable. Craniofacial Surgery Is Teamwork It is obvious from the congenital craniofacial malformations presented in this chapter that management of these malformations should involve a craniofacial team, including but not limited to a pediatric neurosurgeon, craniofacial plastic surgeon, oral/ maxillofacial surgeon, pediatrician, geneticist, and nurse specialist.
The anterior pins should be placed immediately above the eyebrows to take advantage of the thick lateral supraorbital buttress250 and laterally to avoid injuring the supraorbital and supratrochlear nerves allergy shots natural alternative discount promethazine 25 mg on-line. The torque used for pin tightening should be between 2 and 4 inch-lb, depending on the size of the child. For children 10 months to 3 years of age, "tiny tot" haloes are available with a small ring and up to 10 small pins that should be only finger-tightened. As a result of the viscoelastic properties of the skull, the pins frequently loosen up to 4 inch-lb after the vest and uprights are attached to the ring, and they must be retightened to the correct torque 24 hours later. If a loose pin is discovered 2 to 3 weeks after insertion, management depends on the age of the patient. Garfin and colleagues found that with 6 inch-lb of torque, the halo pin only partially penetrates the outer table of the adult skull and there is usually a solid margin of cortical bone to allow safe retightening. Accelerated osteoclasis around the pin site softens the bone so much that retightening can cause full-thickness penetration and an intracranial abscess. Baum and coworkers reported a 31% incidence of pin infection in children versus 6% in adults. If the infection is mild and superficial, with only minimal surrounding scalp erythema and drainage, and the pin remains tight, oral antibiotics are prescribed. If the scalp is red and swollen, the drainage becomes copious and purulent, or the child complains of constant local pain or headaches, the pin should be removed and intravenous antibiotics administered to prevent the dreaded cranial osteomyelitis. Direct contact of the ring and posterior uprights with the bedding should be avoided to minimize transmitted flexion stress. We use a large foam wedge to prop up the back of the vest so that the child can recline comfortably with the head and halo ring hanging free and still be able to watch television, read, play board games, and self-feed. Finally, children tend to be very unforgiving if the head position is not adjusted exactly to their liking. Children in traction also tend to thrash about in bed and are at higher risk than if a one-piece orthosis is worn. Thus, for children between 1 and 4 years of age, the halo device is used for immediate stabilization. If the unstable segments in these young children are grossly malaligned, especially when the cord injury is incomplete, the segments should be reduced by fluoroscopically guided manual manipulation under general anesthesia, preferably with electrophysiologic monitoring. Afterward, fine-tuning and maintenance of the reduction can be achieved by adjusting the halo ring. If closed reduction is unsuccessful, the surgeon should proceed with open reduction and simultaneous fusion. For children younger than 1 year, the problems are even greater because halo rings are not designed for such fragile crania. If the fracture is unstable, there is no safe and effective means of emergency stabilization except open reduction and fusion. An appropriate external orthosis (see later) should then be applied in the operating room. Fortunately, unstable cervical fracture-dislocations are uncommon in this age group. Skull caliper traction can be used safely on children from 5 to 12 years old, but with a modified protocol. First, strong sedatives are administered to contain body motions and relax the nuchal muscles. Second, in young children, the forces required for reduction are much less than those needed for adults, and the degree of ligamentous instability is often underestimated. Each increment in weight must be monitored with a lateral x-ray film to guard against overdistraction. However, mechanical dysphagia develops in children when the neck is even slightly extended because of restricted upward movement of the larynx during the pharyngeal phase of swallowing. Thus, the neck should be put in the "military salute" position, in which posterior translation is substituted for extension. For young children, the top-heavy halo bars and vest in effect shift the center of gravity upward, and they must be patiently coached to relearn the basic skills of walking and navigating. Order promethazine cheap online. Gluten Allergy vs. Celiac Disease.
|