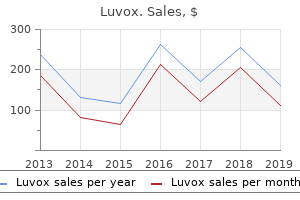
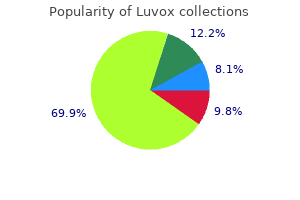
Luvox"Buy luvox 50 mg lowest price, anxiety zone ms fears". By: W. Ressel, M.A., M.D., M.P.H. Professor, Nova Southeastern University Dr. Kiran C. Patel College of Osteopathic Medicine Force duction test under local anaesthetic (should detect entrapment of orbital soft tissues) anxiety vs panic attack cheap generic luvox canada. Reduction and repair 533 Indications include high energy injuries (is the orbital apex involved Ultrasound has been reported as useful for detecting fractures, but is not commonly used. In the interim, patients should be advised not to blow their nose, in order to avoid surgical emphysema. This can result in orbital cellulitis, both a sightand life-threatening condition if untreated. Accept if minimal, to avoid risks of surgery (especially in medically compromised and those on asprin/anticoagulants). The arch is important for cheek projection and may need to be reduced and aligned fully to maintain this. Closed reduction techniques include the following: facial deformity; loss of lower eyelid support; ocular dystopia; limitation of mandibular opening; sensory nerve deficit thought to be due to nerve compression. Timing of treatment depends on the degree of swelling and the general condition of the patient (notably any head or ocular injuries). However, significant swelling may interfere with accurate clinical assessment, both as an indication for treatment (do not just look at the x-ray), and an on-table assessment (is this adequately reduced Furthermore, swelling may be exacerbated by surgical manipulation, so care should be taken if there is any proptosis. All of these involve making an incision somewhere on the patient and could therefore technically be argued as open techniques. This is based on the concerns regarding masseteric and other forces acting on an unsupported reduction over the ensuing weeks. However, this is still a matter of personal preference for each surgeon and closed techniques still have an important role to play in management. These scars may be more noticeable, contraction can distort the lower eyelid, there is a risk of injury to the infraorbital nerve and the fixation is the weakest of all the fracture sites. This is only required occasionally and in significantly telescoped arches, but it does necessitate a posterior approach (preauricular or cutaneous incision). Careful assessment is necessary, even if not telescoped it may be bowed laterally and needs at least digital reduction. In many cases, this may be the only procedure required, if (1) and (2) are not significantly displaced. A step-wise approach is therefore needed and patients need to give informed consent appropriately. Alternatives include the following: Isolated arch fractures 537 (a) (b) (c) (d) (e) (f) 7. Some surgeons prescribe steroids (dexamethasone/methylprednisolone) to reduce post-operative orbital swelling. This is certainly quick, but is a blind procedure with risks to both eyes if incorrectly performed. As patients wake up, they may be initially agitated and the repaired site must be protected from inadvertent injury. Various ways of achieving this are possible, but having the site clearly marked and an alert recovery/ward nurse go a long way to (a) (b) (c) (d) 7. Swelling and bleeding behind the globe can occur, which unrecognized can result in loss of vision. Careful observation of the eye is therefore important, at least until the patient is awake. Antibiotics and steroids may be continued for a variable time and patients should be advised not to blow their nose. For this reason, the eye is put under careful observation, usually until the next day, although they can probably be stopped when the patient is fully awake. Progressive pain, deteriorating vision, proptosis and ophthalmoplegia are the main signs to check. The key to urgency of treatment is the visual acuity, if the vision is normal, decompression is not required. This beam is further passed through a series of focusing lens to reduce its diameter and increase its intensity and energy to make it suitable for clinical applications anxiety symptoms lightheadedness order discount luvox line. The differing types of laser now available is determined by the active (lasing) medium producing the beam (Table 3. The lasers used in maxillofacial surgery are often delivered to the tissues via optical cables or through mirrors in an articulated arm and are dependent on the wavelength and power of the laser beam. Further, the power, focus and duration that the beam dwells in a particular spot also influences the tissue effects (focused beam, incision; defocused beam, vaporize at high power, coagulate at low power). The wavelengths, target chromophores and principle uses of the commonly used lasers in maxillofacial surgery are highlighted in Table 3. In general, there is very little inflammation associated with laser wounds with a resultant decrease in pain and scarring. This is thought to be due to the denaturation of proteins, including the inflammatory mediators, with subsequent underestimation by the body of the damage caused by the laser. Photothermal effects are due to the production of heat from the absorption of laser energy; photochemical effects are due to changes in the chemical composition of the tissue resulting from the absorption of laser light and photomechanical effects results from the target area being mechanically destroyed by laser absorption. Selective photothermolysis is the ability to achieve temperature-mediated localized injury to the target tissue through a specific chromophore, while minimizing damage to the surrounding tissue, and is dependent on the use of a laser with an appropriate wavelength, energy fluence and pulse duration. Thermal relaxation time is defined as the time required for a given heated tissue to lose 50 per cent of its heat through diffusion and therefore significant thermal diffusion (thermal damage) can be minimized if the duration of the laser pulse is shorter than the thermal relaxation time of the target tissue. The clinician using the laser is responsible for the safety of the patient and the staff. Local policies should, however, be in place to allow use of lasers by only trained clinicians, in a safe laser environment staffed by a trained support team. These operational aspects are often overseen by laser protection supervisors and laser protection advisors in the hospital. The clinician should demonstrate appropriate training, understanding and experience with lasers in addition to being aware of the local safety guidelines. The supporting team, which usually includes a senior nurse, prepares the theatre, checks and starts up the laser and assists with the setting during its use. A safe environment involves the creation of a laser lighttight envelope to the theatre in addition to provision of a regularly serviced and inspected laser machine. The access should be limited to essential personnel instructed in laser safety and doors should be locked and all windows and ventilation pathways covered with shutters. Clear warning with illuminated signs should highlight that a laser procedure is in progress and local safety rules apply. These signs are usually interlocked with the electrical supply of the laser machine and illuminate automatically when the power is switched on. Some hospitals have interlocks on the doors, which inhibit laser emission if the door is opened and interrupts clinical procedures. In these instances, it would be sensible to have additional door locks to prevent interlocks cutting the laser emission. The areas surrounding the operative site are protected by a thick layer of saline-soaked gamgee, in which a small hole can be cut to allow access to the target site. A laser grade smoke evacuation system (high flow; two stage filtration; filtration efficiency >99. Antiviral prophylaxis (famciclovir, valacyclovir) should be instituted in this group of patients. Clinical staff and patient protection All the staff in the theatre, including the surgeon, should wear eye protection designed for the particular laser in use. These are designed to provide protection from accidental exposure and are not intended to allow direct viewing of the laser beam! It is essential that the hand piece is not waved around carelessly when the laser is switched on. When active, it should only be aimed at the operation site and at all other times should be switched to the safe standby mode. The support staff in charge of the machine should always keep an eye on the clinician and should switch to standby mode if the laser is being pointed away from the operative site. The key areas of patient safety in maxillofacial surgery relates to the airway, eyes and sites adjacent to the target. Cheap luvox 50 mg online. (*Childhood Anxiety* Symptoms and Solutions).
The horizontal cut can now be made with a retractor situated medially to protect the peritoneum anxiety psychiatrist buy discount luvox 100 mg online. Bone harvesting the point at which bone harvest should commence along the length of the ilium is dependent on three factors: 1 the quantity of bone required: this flap will reach the contralateral ramus with total mandibular reconstruction, but the entire length of the ilium that can be harvested with the muscle and pedicle will be required. Note that the two incomplete osteotomy cuts that will be greenstick fractured later. Operation 239 Once it has been ascertained that the flap including the bone is bleeding, attention should be drawn to the donor site, most of which can be closed before detaching the pedicle. To aid this, a series of holes are made approximately 1 cm apart along the inner and outer cortex of the bony defect in the ilium. It is recommended to use 1 or 1/0 nylon sutures and temporarily hold them with artery clips until all the sutures have been placed before tying the knots. A piece of nonresorbable mesh should be trimmed to the size of the internal oblique defect. A suction drain with a minimum intraluminal diameter of 3 mm should be placed over this layer and an epidural catheter teased through one of the sutured muscle layers. Both of these devices should be secured to the skin with a suture immediately after introduction. Closure of the muscle layers medial to the ilium has to be delayed until pedicle division. If detached, the inguinal ligament is sutured to the ilium and the external oblique muscle is closed to itself medially and to the gluteus medius muscle laterally. Even if a large skin flap has been harvested, direct skin and subcutaneous tissue closure is assured. Insetting and anastomosis the bony component of the flap should be adjusted with a saw if required, rotary instruments are not recommended in case the pedicle is snagged and torn. In contrast to the fibula, the iliac bone is contoured using opening osteotomies with simple splitting of the bone prior to spreading the bone around the cut. The muscle and skin should just be tacked in place to orientate the pedicle, and the anastomosis prepared and carried out at this stage. This allows no interruption of flow through the artery once this anastomosis is complete. It may be that the heparin prevents fibrin degradation products in the previously ischaemic tissue, setting off the clotting cascade Division of the pedicle Final dissection of the proximal pedicle should be undertaken and the artery and vein divided and ligated. The transversalis and parts of the iliacus are sutured into these holes with a round body needled 1 or 1/0 nylon suture. It is recommended to temporarily hold the sutures with an artery clip until all the sutures have been placed before tying the knots. After the flap is running, the internal oblique muscle is sutured into the intraoral defect. Some muscle trimming may be required but, although the flap may appear very bulky at this stage, it is likely to shrink back in a matter of weeks and certainly after radiotherapy. Violation of the thin transversalis muscle to produce herniation of pre-peritoneal fat is always a possibility but can be closed. Snagging of the pedicle with a rotary instrument is possible and potentially disastrous; use of these instruments should be minimized in this operation! For venous monitoring, the colour of the flap, which will obviously appear dark if engorged, is useful. Stabbing the muscle may be useful, bright red blood should flow rapidly and if individual muscle fibres can be seen it probably signifies the flap is not working. A Doppler probe sutured around the flap side of the venous anastomosis may also be helpful. None of these methods is 100 per cent reliable, and it is fair to say this is a difficult flap to monitor. Transillumination It is important to confirm the position and ensure that the stomach is in direct contact with the abdominal wall without any intervening tissue anxiety attack symptoms yahoo buy luvox cheap. This is done by transillumination of the anterior abdominal wall with the light from the endoscope. When choosing an appropriate type for an individual patient, particular consideration should be given to the following: How easy it is to accidentally displace/remove the tube (particularly for confused patients). The normal life span of the tube and hence frequency of necessary replacement (which could be of great importance for an otherwise fit patient requiring longterm nutritional support, but will be less relevant for temporary feeding or when the prognosis is poor). The procedure required for replacement (some require repeat endoscopy, whereas others can be replaced percutaneously in the community). They can be placed either as a primary procedure or to replace a previously established tube). Pushing the small diameter needle used to infiltrate the local anaesthetic through to the stomach until it is visible on the camera allows a final safe confirmation of the site and angle of insertion of the trocar/cannula apparatus. With a jab from the wrist, the tip will pass through the wall into the stomach, which is being kept distended by the endoscopist with continuous air insufflation in order to avoid trauma to the opposing wall. The endoscopist then passes the snare down the biopsy channel of the endoscope and over the trocar/cannula closing it gently. The trocar can then be removed leaving the cannula in place and the insertion thread (or wire) passed through the cannula until about 10 cm lies within the gastric lumen. The snare is then loosened from the cannula and slipped off, to be tightened securely on to the insertion thread. The endoscope and snare are then removed together, trailing the thread all the way back out of the mouth. Some types can be removed simply by cutting off the external portion and pushing through the internal portion, allowing it to pass naturally. There is a small risk of impaction or perforation when using this technique though and endoscopic removal may be preferable. In the push method, a strong guidewire is used in place of the insertion thread, but is placed in the same way. In the peel-away sheath method, the optimal site is assessed endoscopically and the stomach inflated. A needle is then inserted into the stomach and a short guidewire passed through it. The needle is removed and a dilating introducer with an outer peel-away sheath is inserted. The introducer is removed, leaving the sheath through which a Foley-type balloon catheter is passed. Pulling the gastrostomy into position the endoscopist ties the tapered end of the gastrostomy tube to the insertion thread at the mouth and the assistant then pulls the abdominal end of the thread until the attached tube abuts the cannula (which can be felt as the thread stops running freely). The remaining length of the tube is then pulled through until the internal bumper is felt to come into contact with the stomach wall. The tube can then be cut to a sensible length and the external bolster and feeding line attachment threaded on. It is vital that the external bolster pulls the tube tightly enough for the stomach to appose the abdominal wall in order for a fistulous tract to form, but not tightly enough to cause ulceration or tissue necrosis (see Table 4. Opinion is split as to whether it is necessary to repass the endoscope to check the bumper position internally. Patients should receive hourly temperature, pulse and blood pressure observations for 6 hours post-procedure and the site should be inspected the following day for any signs of infection. Variations in body habitus, hiatus herniae and abdominal viscera can make the insertion procedure challenging and both endoscopist and assistant require skill and training. The ideal opportunity for insertion in maxillofacial patients will often be while they are under general anaesthetic either for assessment or for definitive surgery. It may be that the delay and discomfort associated with a visit to the endoscopy unit could be avoided if appropriately trained maxillofacial surgeons were able to perform the procedure at this time. Prospective, randomised, double blind trial of prophylaxis with single dose of co-amoxiclav before percutaneous endoscopic gastrostomy.
|