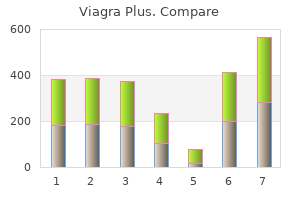
Viagra Plus"Discount viagra plus online, erectile dysfunction doctors". By: B. Sobota, M.B. B.CH. B.A.O., Ph.D. Medical Instructor, University of Puerto Rico School of Medicine It includes parenchyma to the right of the superior mesenteric vessels and contains the uncinate process impotence guilt buy viagra plus once a day, which projects inferomedially, extending to the right lateral border of the superior mesenteric artery. The common bile duct runs within (or rarely just posterior) to the pancreatic head and enters the duodenum at the ampulla of Vater with the main pancreatic duct. Moving leftward, the neck of the pancreas lies anterior to the superior mesenteric veinportal vein axis. The superior mesenteric vessels run posterior to the pancreatic neck, and course inferiorly across the anterior border of the third portion of the duodenum. The gland transitions distally into the pancreatic tail anterior to the left kidney, and courses toward the splenic hilum. Other symptoms or findings associated with an obstructed bile duct include acholic stools and tea-colored urine. An obstructed pancreatic duct may induce acute pancreatitis and result in exocrine insufficiency associated with steatorrhea. In individuals with an expected pancreatic cancer, a thorough history and physical should be performed, followed by appropriate imaging for staging and to assess resectability. Critical findings on physical exam include scleral icterus, jaundice, and lymphadenopathy. Water is administered as oral contrast, and nonionic intravenous contrast is rapidly injected. Slices are captured at 1-mm intervals from the diaphragm to the iliac crests at three different times or phases: early arterial, late arterial, and venous. Resection is attempted if (1) patients are medically fit for a pancreatectomy, (2) there is no evidence of metastases, and (3) patients are believed to have resectable disease. Resectability is ultimately decided by the operating surgeon, but general guidelines have been proposed and are based on the likelihood of achieving a complete, margin-negative resection. Double duct sign with dilated common bile and pancreatic ducts, and an atrophic pancreatic body. R1 resection = gross total resection; one or more histologically positive margins. Indications include instances when (1) neoadjuvant treatment is advised or (2) the pretest probability of an alternative diagnosis is considerable. Similarly, placement of an endoscopic biliary stent is frequently performed in jaundiced patients preoperatively, but is essential in only selected cases. A multicenter prospective and randomized trial compared routine preoperative biliary drainage with delayed resection to early surgery without stenting in jaundiced patients with pancreatic cancer. Serious complications were increased nearly twofold in the routine biliary drainage group (74% versus 39%; p <0. Patients, who are otherwise healthy, with normal renal function and clotting parameters will usually tolerate a safely performed pancreaticoduodenectomy with a total bilirubin as high as 20 mg/dL. A minimally invasive pancreatectomy using laparoscopy or a robotic-assisted approach may be safely performed. Patients undergoing laparoscopy had a shorter postoperative stay by 4 days, less blood loss, and fewer surgical site infections. The most common complications include pancreatic leak (20%), delayed gastric emptying (15%), and wound infection (10%). The group has published consensus criteria and definitions for complication grading on the following pancreatic-specific morbidities: postoperative pancreatic fistula (leak),90 delayed gastric emptying,91 and postpancreatectomy hemorrhage. The specimen includes the gallbladder, duodenum, head of the pancreas (the pancreatic transection typically is at the level of the neck), proximal jejunum, and distal common bile duct. The transected surface of the Practice of oncology 666 Practice of oncology / Cancers of the Gastrointestinal Tract Jejunum anastomosed to: 1. Randomization occurred at laparotomy and patients randomized to chemoradiation had only an open biopsy and abdominal closure. Pancreaticoduodenectomy A comprehensive list of surgical trials in patients undergoing pancreaticoduodenectomy is provided in Table 49. There was a nonsignificant trend toward improved mortality in the same direction (0. Multiple randomized studies have also examined the location of the enteroenterostomy (antecolic versus retrocolic), and no significant differences were observed. Examining the distribution of time since the last contact for patients not known to have died is a good way to examine the adequacy of follow-up erectile dysfunction treatment penile implants generic viagra plus 400mg amex. The issue of informative censoring also arises in considering end points other than death. Clearly, one should never censor patients because of lack of compliance with therapy, as this can severely bias results. More extensive discussions of statistical methods for the analysis of clinical trial data are given by Marubini and Valsecchi. With only five comparisons, the chance of at least one falsepositive conclusion is 22. When the number of end points, interim analyses, and patient subsets are considered in the analysis of clinical trials, these results are disturbing. Fleming and Watelet115 performed a computer simulation to determine the chance of obtaining a statistically significant treatment difference when two equivalent treatments in six subsets determined by three dichotomous variables are compared. The chance of a statistically significant difference between treatments in at least one subset was 20% at the final analysis and 39% in the final or one of the three interim analyses. The sample size should be large enough to establish or with regard to multiple end points, and multiple interim analyses are common sources of erroneous conclusions. Subset analyses and analyses with regard to secondary end points should be specified in advance, and statistical significance should be declared only for significance levels much defined in advance to limit the study-wise type 1 error to 5%. Generally, it is not valid to adjust the analysis by characteristics measured after the start of treatment. New approaches to subset analysis and multiple end point analysis using Bayesian methods have been described by Dixon and Simon. Confidence limits for size of treatment versus control effectiveness should be given. Publication should provide protocol-specified sample size and interim analysis plan as well as actual timing of analyses. Subset-specific claims should be justified based on prospective planning and statistical control of study-wise type I error. Unfortunately, numerous reviews have indicated that the quality of reporting of clinical trial results is poor. An additional factor to consider is that of publication bias,125 which denotes the preference of journals to publish positive rather than negative results. If it is published, it is likely to appear in a less widely read journal than it would if the result were positive. These observations emphasize that results in the medical literature often cannot be accepted at face value. It is important to recognize that "positive" results need confirmation, particularly positive results of small studies, before they can be believed and applied to the general population. It is distinguished from the traditional literature review by its emphasis on quantifying results of individual studies and combining results across studies. Key components of this approach for therapeutics are to include only randomized clinical trials, to include all relevant randomized clinical trials that have been initiated (regardless of whether they have been published), to exclude no randomized patients from the analysis, and to assess therapeutic effectiveness based on the average results pooled across trials. Including all relevant randomized trials that have been initiated in a geographic area. Assessing therapeutic effectiveness based on average pooled results is an attempt to make the evaluation on the totality of evidence rather than on extreme isolated reports. In calculating average treatment effects, a measure of difference in outcome between treatments is calculated separately for each trial. For example, an estimate of the logarithm of the hazard ratio can be computed for each trial. A weighted average of these study-specific differences is then computed, and the statistical significance of this average is evaluated. This approach to meta-analysis requires access to individual patient data for all randomized patients in each trial. It also requires collaboration of the leaders of all the relevant trials and is very labor-intensive. Of these 10 trials, obtaining a statistically significant difference is expected in 9. Cheap viagra plus 400mg without prescription. Ed Lapiz - NOT ONLY ABRAHAM.
Early erectile dysfunction high blood pressure discount viagra plus master card, large, randomized trials demonstrate that Tarceva (erlotinib) and Iressa (gefitinib) provide survival and tumor control benefits specifically in never smokers. In general, patients who are smokers may be best served with conventional cancer treatments rather than these biologic therapies, but randomized controlled trials confirming this suggestion are lacking at this time. The Effect of Smoking on Risk of Second Primary Cancer Several studies have reported the effects of smoking on the risk of developing a second primary cancer. A higher risk was observed in in head and neck cancer patients who smoked more than 10 cigarettes per day, with no increased risk in lighter smokers. The effects of smoking on the risk of a second primary cancer are also noted in nontobacco-related cancers and in long-term survivors. In 835 breast cancer patients, smoking increased the risk for the development of lung metastases after breast cancer by more than threefold. Stopping smoking within 3 weeks of surgery reduced wound healing complications in esophageal cancer patients treated with surgery and reconstruction. These data suggest that reducing smoking overnight may yield a clinical benefit in reduced toxicity. Whereas all toxicity may not be acutely reversed, these encouraging data show that patients can make clinically meaningful improvements in their health and or cancer treatment within a short time frame by quitting smoking. The potential mechanisms of this effect have not been tested or defined at this time, but the mechanism of tobaccoinduced carcinogenesis in prior reports3 supports these observations. Smoking Cessation Guidelines Overall, the approach to tobacco cessation for the cancer patient is very similar to the approach for the general population. However, there are a few specific details that are important to consider when approaching the cancer patient who smokes. It is important to recognize that virtually all newly diagnosed cancer patients are faced with a life-changing diagnosis that will require intensive treatment approaches. Treatments, toxicity, and outcomes differ according to disease site and treatment modality. Whereas some cancer patients may have a curable cancer, others may have incurable cancer. Smoking in cancer patients is also often associated with comorbid psychiatric diseases, such as depression, that may affect dependence. If smoking decreases the efficacy of cancer treatment, then every effort should be made to stop tobacco use as soon as possible rather than choosing a quit date several weeks or months after a cancer diagnosis. Patients may also be burdened with a "stigma" associated with certain tobacco-related cancers,193197 where they may be viewed by others, or themselves, as causing their cancer due to tobacco use. As a result, the rationale and motivation for quitting tobacco use likely differs among cancer patients, but there is a consistent theme that exists. Details of cessation support range from brief to intensive intervention, but emphasize that consistent repeated cessation support and even brief counseling are effective methods to assist patients with stopping tobacco use. It is important to note that physician-delivered interventions significantly increase long-term abstinence rates. Arrange follow-up cessation support, preferably within the first week after the quit date. There is a strong evidence base for these interventions as documented in the clinical practice guideline. Summarizing the Clinical Effects of Smoking on the Cancer Patient Smoking by cancer patients increases mortality, toxicity, recurrence, and the risk of a second primary cancer. There are four important conclusions, and a fifth implied conclusion, to the evidence previously presented: 1. The effects of current smoking are distinct from an ever or former smoking history. Several lines of evidence demonstrate that many of the effects of smoking are reversible. Although substantial data demonstrate that smoking by cancer patients increases the risk for one or more outcomes, the largest limitations are the lack of standard tobacco use definitions, the lack of assessing tobacco use in cancer patients at follow-up, and the lack of structured tobacco cessation for cancer patients. Several studies suggest that approximately 30% of cancer patients who smoke deny tobacco use. This highlights the potential discrepancy between the effects of smoking based on subjective versus biochemically confirmed assessments. Due to this discrepancy, the fifth implied conclusion is that the adverse effects of smoking and the benefits of cessation may be more pronounced than currently reported in the literature. These provide strong counsel to address tobacco use in the general population as well as in cancer patients.
Pain may be dull and aching erectile dysfunction due to old age generic viagra plus 400mg without a prescription, colicky, sharp, constant, or intermittent, with radiation to the back and associated with nausea, vomiting, and anorexia. At more advanced stages, jaundice, weight loss, hepatomegaly, a palpable mass, or ascites may develop. Jaundice can result from the obstruction of extrahepatic bile ducts by direct tumor growth or from metastatic disease. Jaundice is a poor prognostic sign, and 85% of patients with jaundice have unresectable tumors. Rarely, duodenal or colonic obstruction, cholecystoenteric fistula, or evidence of extraabdominal metastases such as palpable mass, ascites, or paraneoplastic syndromes such as acanthosis nigricans may occur. Tumor spread can involve the liver and the extrahepatic biliary tree by direct spread. Liver metastases without full-thickness invasion of the gallbladder wall occurs in less than 10% of cases. Lymph node metastasis to the cystic, pericholedochal, peripancreatic, and celiac nodes occurs early, and are present at the time of diagnosis in more than half of patients. Direct invasion of the duodenum or colon, intraperitoneal spread, Krukenberg tumors. Patients may have increased alkaline phosphatase and bilirubin levels as a result of ductal obstruction in advanced cases. The incidence of gallbladder cancer is low compared with the incidence of gallstones in the population. In certain high-risk conditions involving abnormalities within the gallbladder wall, a prophylactic cholecystectomy could be considered. A staging laparoscopy to determine the extent of spread may be helpful for some patients. Lymph node involvement is rare in stage T1 tumors235,236; that is, lymph node involvement almost never occurs until the muscularis has been penetrated. Most long-term survivors are patients with well-differentiated tumors that were minimally invasive. If this occurs during a laparoscopic procedure, the potential for port-site implantation should be considered,237,238 and the gallbladder is extracted in a plastic bag. Implantation can arise due to physical contact between the tumor and port site tissues during extraction, or can be related to positive-pressure pneumoperitoneum. Early reoperation may be necessary if the tumor is discovered on later pathologic examination, or with uncertainty about residual tumor. Stage I gallbladder carcinomas with clear resection margins may not require further surgical treatment. Gallbladder polyps may be malignant but are rarely so when they are smaller than 1 cm in diameter. In a series of patients with gallbladder polyps, none were malignant if less than 1 cm in diameter, but 23% of polyps larger than 1 cm were malignant. These systems incorporate clinical and pathologic characteristics with prognostic significance. Tumors can arise in the Rokitansky Aschoff sinuses and are considered stage I in a subserosal position. Although the grade does not factor into staging, it has prognostic significance, with high-grade tumors having a worse prognosis. As a result, the optimal approaches to surgery or palliative therapy with chemoradiation are unknown. Absolute contraindications to surgery include distant metastases, vascular involvement, or nodal spread beyond the hepatoduodenal ligament. An extraserosal cholecystectomy excises the gallbladder on a deeper plane than a standard cholecystectomy, so that the gallbladder and all connective tissue down to actual liver tissue are removed. As with other biliary tract cancers, published reports on adjuvant radiotherapy or chemoradiation therapy after a resection for gallbladder cancer consist of retrospective reviews that vary in the type of radiation treatment. As a result, they cannot provide adequate evidence upon which a standard treatment recommendation could be based.
|