Bisoprolol Fumarate"Order bisoprolol 5mg line, hypertension means". By: X. Pakwan, M.B.A., M.B.B.S., M.H.S. Clinical Director, UT Health San Antonio Joe R. and Teresa Lozano Long School of Medicine Once the islets are received blood pressure chart senior citizens purchase bisoprolol online pills, they are infused through a surgical or, radiological procedure. The implantation site is usually the hepatic parenchyma through the portal system of the recipient. The surgical procedure is performed after the conclusion of the kidney transplant through injection of the islets in the portal system by opening the peritoneum and catheterization of an ileal vein. The percutaneous approach is done by a minimally invasive procedure requiring interventional radiology technology. The portal vein is reached by a percutaneous catheter placed under ultrasound or angiographic guidance. Combined Kidney-Islet Transplantation 379 the radiological infusion of the islets can be performed few hours after the end of the kidney transplant or at long time after the operation, as for the islet after kidney transplant or in the case of subsequent islets infusions in patients just transplanted with islets. Recently other implantation sites have been proposed in the clinical setting, like bone marrow (Cantarelli et al. Complications related to islet transplantation the procedure of islet transplantation proved to be very safe, especially when compared with the transplant of the whole pancreas. Ower and collegues in 2003 showed that the most severe complications occurred in this case were intraperitoneal haemorrhages; anyway these were generally treated conservatively. The exact cause of bleeding in each case is often difficult to determine; however the peri-operative use of heparin to prevent portal thrombosis likely plays a role. The use of fibrin tissue sealant and embolization coils in the hepatic catheter tract seems to be effective in minimizing the bleeding risk. Another complication related to the intrahepatic islet transplantation procedure is the insurgence of portal hypertension that can occur acutely during the islet infusion especially 380 Understanding the Complexities of Kidney Transplantation in the case of subsequent infusions (Casey et al. The portal pressure however generally normalizes after the acute phase of the procedure. Branch portal vein thrombosis was also frequently reported in the past; anyway this complication is generally limited and controlled with appropriate anticoagulation therapy. Actually the use of purer islet preparations, greater expertise in portal vein catheterization and new radiologic devices (catheters medicated for anticoagulation) will constantly reduce the risk of portal vein thrombosis although it will never be completely removed. A complication frequently reported is even the post-transplant elevation of liver enzymes but this is usually temporary and heals without further intervention. Successively the onset of focal steatosis in patient after islets transplantation was studied by sonogram (Maffi et al. These authors reported that signs of steatosis were often observed in patients after islet transplantation with total or partial function of the graft and normal liver function anyway was maintained in all of these. It was even proposed to consider the disappearance of this signs as a early marker of graft dysfunction. Combined kidney-islet transplantation: Indications the American Diabetes Association guidelines. However since the procedure of pancreas transplantation has an high incidence of mortality and morbidity (Gruessner et al. Considering the much lower incidence of complication after islets transplantation several kidney-pancreas centers have also started programs of kidney-islets transplantation basing on the fact that these two procedures are complementary and suitable for patients with different features. Although the success of pancreas transplantation in term of graft survival is higher than islet transplantation with 80% of insulin-independency after 3 years. Actually the patient selection for either two therapeutic options is performed after a careful evaluation of possible advantages and disadvantages, with special regard to age and comorbidities. Patients at high risk of intraoperative complications are preferentially assigned to the less invasive procedure of islet transplantation, while younger and healthier patients are generally addressed to pancreas transplantation (Gerber et al. In particular kidney-islets transplantation is preferred to kidney-pancreas for patients over 50 years of age or with severe macroangiopathy. Islet transplantation should also be Combined Kidney-Islet Transplantation 381 considered for all the patients who underwent kidney-pancreas tranplantation and have functioning pancreatic graft removed for complications as recidivant anastomotic leackage. In this case the possibility to use the removed pancreas for the islets isolation procedure has to be considered.
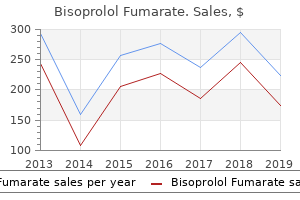
Pulmonary edema is a common complication in patients who are fluid over loaded prior to the institution of treatment hypertension organ damage generic bisoprolol 10mg. Consequently, chest radiographs are routinely obtained before treatment begins to exclude preexisting pulmonary edema or heart failure. Increased risk is associated with overhydration, twin gestation, and use of steroids. Generally speaking, radiation is best tolerated by the patient if given in smaller doses, over a long period of time, and to a single lung or a small lung region. For unilateral radiation with fractionated doses, radiographic findings of radiation pneu monitis are seldom detected with doses below 3,000 cGy, are variably present with doses between 3,000 and 4,000 cGy, and are nearly always visible at doses of 4,000 cGy. Its likelihood is increased by a second course of radiation, the withdrawal of corticosteroid treatment, and the use of concomitant che motherapy. Radiographic findings of radiation pneumonitis are usually not associated with symptoms, although low-grade fever, cough, and dyspnea are present in some patients. Radiation Pneumonitis Pulmonary abnormalities related to radiation injury have been divided into early and late manifestations. The early stage of radiation lung injury, referred to as radiation pneumonitis, occurs within 1 to 3 months after radiation therapy is com pleted and is most severe 3 to 4 months following treatment. Depending on the severity of lung injury, these abnor malities may resolve completely, but more often they undergo progressive organization, leading eventually to fbrosis. B A: Patchy areas of ground-glass opacity are visible in a paramediastinal dis tribution following mediastinal radiation. B: the areas of abnormality are nonanatomic but have straight margins cor responding to the radiation ports (arrows). Histologically, dense fbro i sis with obliteration of lung architecture and traction bron chiectasis are present. Patients can present with radiation fibrosis without a previous history of acute pneumonitis. Abnormalities are typically nonanatomic and do not tend to respect normal lung boundaries such as lobar fissures or lung segments. Volume loss can be seen; this is due to obstruction of bronchioles by inflammatory exu date, loss of surfactant, or both. The development of radiation fibrosis can be recognized by the appearance of streaky opacities, progressive volume loss, progressive dense consolidation. This gives the abnormal lung regions a characteristically straight and sharply defned edge. Pathogenesis of pulmonary edema during interleukin-2 therapy: correlation of chest radiographic and clin ical findings in 54 patients. Although pleural thickening is a common manifestation of radiation, pleural effusions are uncommon. Effusion related to radiation typically develops within 6 months of treatment, in conjunction with radiation pneumonitis, and resolves spontaneously. Mediastinal lymph node calcification, particularly after radiation of lymphomas, the development of thymic cysts, pericarditis, and cardiomyopathy may also be seen. Inhaled brosis and dis Profusion the number of small rounded or irregular opacities is indi cated by the term dusts may be toxic, resulting in ability. Inhala tion of organic dusts results in hypersensitivity pneumonitis (see Chapter 16). This system provides a semiquantitative method for assessing the type and extent of abnormalities present. Classi cations using this system are nonspeci c, however, and it has little role in diagnosis. Furthermore, this system is complicated and dif cult to remember unless used on a regular basis. A combination of letters and numbers is used to indicate the type and extent (profusion) of opacities present. One or a cluster of several opacities >10 mm to 5 cm Larger or more numerous than A, not larger than the right upper lobe Larger than B Absent or less profuse than 1 Definitely present but few in number (normal lung markings are still visible) Numerous small opacities (normal lung markings partially obscured) Very numerous small opacities (normal lung markings usually obscured) Small irregular opacities are linear or reticular in appear ance and are indicated as s, t, or u according to their thick ness. These are dassi- Profusion (of small opacities) 0 1 2 ed as A if a single lesion or duster of several opacities is more than 10 mm, but 5 cm or less in diameter. Buy genuine bisoprolol line. The Only Blood Pressure and Arterial Health Monitor.
Diagnosis is by exclusion; malignant mesothelioma must be considered in the differential diagnosis yaz arrhythmia discount bisoprolol 5 mg mastercard. Diffuse pleural thickening usually rep resents a synthesis and fusion of thickened visceral and pari etal pleural layers, and it is usually related to the presence of prior asbestos-related benign pleural effusion. Mesa shaped Often appear as high attenuation Calcified in 15%-20% of cases Parietal pleural thickening may be seen without plaques Visceral pleural thickening Lateral lower lobes May be associated with rounded atelectasis Radiographic Findings of Pleural Disease Although plain radiographs may be diagnostic of asbestos related plaques in some patients, they are only about 10% to 40% sensitive in detecting pleural plaques. Pleural plaques are usually visible in the lower half of the thorax and may be seen en face or in pro le along the lateral pleural surfaces. Because they are often posterolateral in location, bilateral oblique views are often advantageous in demonstrating their presence. In pro le, they are often visible internal to ribs, up to 1cm in thickness, and sharply contrasted with adjacent normal pleura. They are calci ed in 10% to 15% of cases; diaphrag matic plaques are most often calci ed. En face plaques are dif cult to recognize as such unless calcied and may mimic lung nodules. Focal or diffuse thickening of the ssures may also be seen, indicative of visceral pleural disease, but is less common. Pleural effusion occurring as a result of asbestos exposure has no distinguishing characteristics. Diffuse pleural thickening appears as a diffuse or con centric increase in pleural thickness. It is often considered to be present if pleural disease continuously involves at least one quarter of the chest wall. These occur in a distribution similar to that of plaques, involving the lower portion of the postero lateral thorax, but are usually longer, have tapering margins, are smooth and symmetrical, and are sometimes seen as lower in attenuation than soft tissue. They are the most common and the most characteristic feature of asbestos exposure. They are composed of dense brous tissue and contain asbestos hers, and calci cation is common. Plaques nearly always involve the parietal pleural surfaces and are frequently seen overlying ribs in the posterolateral thorax and in relation to the domes of the diaphragms. Thin areas of focal parietal pleural thickening without thick plaques may be seen early in the course of disease in patients with asbestos exposure. Visceral Pleural Thickening Visceral pleural thickening may occur, usually along the lat eral pleural surface of the lower lobes. Benign Exudative Pleural Effusion Benign exudative pleural effusion can be an early manifestation of asbestos exposure, being the only nding present in the rst 10 years after exposure; it occurs in 3% of exposed individuals. A similar linear density seen between the ribs (small arrows) is normal and represents the innermost intercostal muscle. Thickened pleura measuring as little as 1 to 2 mm can be readily diagnosed in this location. In the paraver tebral regions, the intercostal muscles are anatomically absent, and any distinct stripe of density indicates pleural thickening. The presence of bilateral pleural plaques or focal pleural thickening is strongly suggestive of asbestos exposure, particularly when calci cation is also seen. Often, even when not grossly calci ed, asbestos-related areas of pleural thick ening appear denser than adjacent intercostal muscles, likely because of their mineral content. A: Chest radiograph shows geographic opacities (small arrows) overlying the lung bases, representing pleural plaques. Pleural plaques are also visible at the domes of the hemidiaphragms (large arrows). Asbestos-related pleural plaques, rounded atelectasis, and pleural effusion due to mesothelioma. It is unusual to see benign pleural effusion with such marked pleural thickening, and in this case the pleural effusion reflects mesothelioma.
For living donor recipients high blood pressure medication toprol xl buy discount bisoprolol 10 mg, perform a monocyte crossmatch should be useful as may help to detect anti-endothelial antibodies. They tested pre-Tx sera from all consecutive deceased-donor kidney 442 Understanding the Complexities of Kidney Transplantation transplants performed between January 2005 and July 2006 (n=237), 66% had a highimmunologic risk. There is evidence that it is possible to reduce pre-existing circulating alloantibodies in some patients to levels where the antibodies are unable to trigger hyperacute rejections. This does not imply that there are no B lymphocytes with the capacity to restart alloantibody production, but the short-term survival of grafts transplanted in some centres under these conditions is acceptable. Immunosuppressive therapy in high immunologic risk patients receiving cadaveric renal allograft 3. These antibodies have the ability to block a number of adhesion molecules, cytokines, chemokines, among others. Antilymphocyte antibodies have long been an integral part of induction regimens and, nowdays, continue to be used in the management of patients at risk of early rejection. Among the available polyclonal globulin, thymoglobulin, has shown a great efficacy and typically requires between 7 and 10 doses. The reaction of these globulins with some lymphocyte antigens can trigger activation of these cells to release cytokines, which may present with chills, fever and systemic symptoms, mainly with the first dose. Steroids, antihistamines and antipyretics intravenous infusion may prevent these early reactions; polyclonal antibodies will be made through a central venous catheter in at least 6 hours. Side effects in the medium and long term are related to its immunosuppressive effect. Other opportunistic infections may be due to pneumocystis jiroveci and aspergillus, but are related to immunosuppression accumulated by the patient rather than the administration of polyclonal antibodies. Treatment with antilymphocyte globulin and a serum test for Epstein-Barr virus receptor are associated with the risk of lymphoproliferative disorders in renal transplant population. It is indicated for the treatment of patients with chronic lymphocytic leukemia who have been treated with alkylating agents and who have not achieved a complete or partial response. The antigen has been detected in a small percentage (<5%) of granulocytes, but not detected in erythrocytes or platelets. Alemtuzumab does not appear to damage the hematopoietic stem cells or progenitor cells. Further long-term controlled studies are needed to establish the potential benefit in terms of efficacy and safety after kidney transplantation. This molecule appears to be associated with the structure of antigen recognition of T cells. Adverse effects are minor: headaches, fever, fatigue, myalgia, hypotension, sweating, dizziness, chills, chest tightness, wheezing. They all probably are secondary to increased levels of inflammatory cytokines and vasoactive substances and with high velocity perfusion. Anaphylactic reaction and shock can occur in patients with total or partial deficiency of IgA. Another adverse effect is renal dysfunction, because of the content of sucrose or sorbitol which can cause osmotic nephrosis in the proximal tubule. This can be avoided by reducing the osmolarity of immunoglobulin products containing sucrose, using restorative with sterile water instead of saline and lowers the concentration of Igs and sucrose to <9%. Directly inhibits B cell proliferation, induces apoptosis and reduces the production of antibodies. Recent clinical data suggest that the beneficial effects of rituximab may be due to depriving T cells of antigen-presenting cell activity provided by antigen-specific B cells, thus altering effect or functions and inducing a regulatory profile. These data suggest that the beneficial effects of rituximab on autoimmune disease are more likely related to modification of dysfunctional cellular immunity rather than simply a reduction in antibody. Rituximab can be administered in a peripheral vein and, although rare, can cause anaphylactic reactions, which suggests his administration under close monitoring. These problems might limit the benefit of rituximab if were used as the sole treatment, however, it appears that the use of rituximab in combination with other treatments.
|