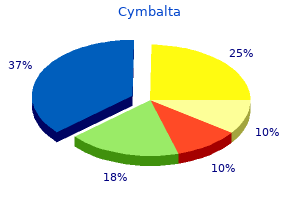
Cymbalta"Buy discount cymbalta 40mg online, anxiety quotes tumblr". By: B. Peratur, M.B. B.CH., M.B.B.Ch., Ph.D. Medical Instructor, The Ohio State University College of Medicine Symptomatic disease ranges from mild anxiety fever cymbalta 20mg, nonspecific symptoms to fulminant hepatitis leading to liver decompensation and death (<1% of cases). The majority of cases of acute hepatitis B are asymptomatic, one third present with jaundice, and <1% present with a fulminant hepatitis. The outcome of chronic hepatitis is dependent on a complex interplay between the virus and the host immune response. Approximately 20% remain with chronic hepatitis, 50% transition to an inactive carrier state, and 30% progress to cirrhosis. The course of acute infection can be viewed in four distinct phases: the incubation phase, before symptoms are present, is notably long, and ranges from 1 to 6 months. This is followed by a pre-icteric or prodromal phase, characterized by the onset of symptoms such as fever, fatigue, anorexia, nausea, vomiting, abdominal pain, jaundice, myalgia, and joint pain. This phase may last for few days to a week and then is followed by an icteric phase manifested by jaundice. Symptoms such as fatigue may persist for a few months even after the resolution of jaundice. Extrahepatic manifestations may be observed with acute hepatitis B and are usually the result of immunemediated phenomena. The arthralgias usually involve the large joints such as the elbows, wrists, knees, and ankles. Polyarthritis nodosa was reported to occur in up to one third of cases of acute hepatitis B [36]. Papular acrodermatitis (Gianotti syndrome) has been reported in children less than 6 years of age with acute hepatitis B. It is characterized by erythematous papules on the face, arms, and legs, with truncal sparing and lymphadenopathy. Essential mixed cryoglobulinemia, membranoproliferative and membranous glomerulonephritis have also been reported to occur with acute hepatitis B. Pathology Acute hepatitis B is characterized by an acute inflammatory response involving the entire liver. The classic histological features of acute viral hepatitis include ballooning degeneration (swollen hepatocytes with enlarged, often multinucleated nuclei and pale-staining cytoplasm), numerous apoptotic bodies and lobular disarray. The lobular disarray results from the combination of cell swelling, cell shrinkage, apoptotic body formation, and cell loss. Inflammatory cells, predominantly lymphocytes and Kupffer cells, are present within the hepatic lobule and portal area. Bile ductular proliferation may be seen but is not a predominant feature of acute hepatitis B. The histological changes associated with acute hepatitis B persist for several weeks after onset. Symptoms when present tend to be mild and nonspecific, such as fatigue and right upper quadrant or epigastric discomfort or ache. Common symptoms of chronic hepatitis may include fatigue, weakness, nausea, and right upper quadrant pain. If the liver disease is more advanced, jaundice, dark urine, itching, and abdominal distension may be present. Pathology the pattern of injury observed on liver biopsy is not specific for chronic hepatitis B. Chronic hepatitis is characterized by inflammation that is located predominantly in the portal areas, with interface hepatitis (extension of inflammation beyond the limiting plate of hepatocytes surrounding the portal area), and less prominent in the hepatic lobule; fibrosis may or may not be present.
However anxiety after eating cheap cymbalta 40mg with amex, a recent randomized study comparing tenofovir or tenofovir and entecavir in 102 patients with adefovir resistance demonstrated similar efficacy for both agents at least in the short term [182]. Tenofovir monotherapy was also shown to be equally effective compared to the combination of tenofovir and emtricitabine in patients with incomplete viral suppression after therapy with adefovir. Among 105 patients with an incomplete response to adefovir, 81% randomized to either tenofovir or tenofovir and emtricitabine achieved complete viral suppression [156]. This study also demonstrates no role for emtricitabine in combination with tenofovir for management of partial response or resistance to adefovir. Tenofovir monotherapy is recommended as salvage therapy for patients who develop antiviral resistance to entecavir. In a randomized trial, tenofovir was shown to be equally effective as tenofovir and emtricitabine for management of entecavir resistance. Combination therapy Combination therapy has been shown to be more effective for management of infectious diseases. In chronic hepatitis B it can lead to a synergistic or additive effect leading to more profound viral suppression and also prevent development of antiviral resistance. Although studies of combination therapy using peginterferon with a first-generation nucleoside analog did demonstrate an additive effect in achieving viral suppression and reducing the incidence of antiviral resistance, the off-treatment responses were similar to that of peginterferon alone, suggesting no benefit of combination therapy. More recently, studies of combination therapy have been conducted with the more potent nucleos(t)ide analogs either together or with peginterferon. After 96 weeks of therapy, the proportion of subjects who achieved viral suppression was not significantly different between patients receiving combination therapy and those receiving entecavir monotherapy (83% vs. For the small minority of children in the immune active phase of infection both interferon and nucleos(t)ide analogs are approved for use in children. However, the decision to Chapter 24: Hepatitis B and D 609 initiate therapy in children should be only undertaken after careful consideration of the benefits and risks of therapy have been thoroughly discussed. Peginterferon alfa-2a is not approved for use in children with chronic hepatitis B but is approved for children with chronic hepatitis C aged 5 years or older and may be considered for use in children due to its more convenient dosing schedule. Efficacy of interferon in children was shown to be superior to no therapy and comparable to that of adults. In the United States, lamivudine and entecavir are approved for children age 2 years and older and tenofovir is approved for children 12 years and older. Entecavir is preferred over lamivudine for children between 2 and 12 years of age due to a lower rate of drug resistance. Significantly more children treated with entecavir achieved the primary endpoint (24. Entecavir was well tolerated with no observed differences in adverse events or changes in growth compared with placebo. Following liver transplantation Liver transplantation for chronic hepatitis B is the only option for patients with decompensated liver disease, despite the availability of potent antiviral therapy. Initial graft and patient outcomes after transplantation were poor, with <50% graft and patient survival at 2 years because of universal graft reinfection [187]. However the introduction of hepatitis B immune globulin and later nucleos(t)ide analogs dramatically improved patient outcomes, with overall survival exceeding 85% at 1 year and 75% at 5 years. At present, the combination of hepatitis B immune globulin and a nucleos(t)ide analog is considered the standard of care to prevent graft reinfection. However, the optimal approach to prevention of graft reinfection has not been clearly defined and there is considerable center-to-center variation in peri- and posttransplant management. Since the availability of nucleos(t)ide analogs, many studies have focused on limiting the use of hepatitis B immune globulin following transplantation because of its high costs. Another approach evaluated was the combination of a nucleos(t)ide analog with lowdose hepatitis B immune globulin. Unfortunately, many of the studies enrolled relatively small numbers of patients, were uncontrolled, and provided limited follow-up. In the absence of a large randomized trial posttransplant management tends to be driven by local transplant center experience. Ideally, the nucleos(t)ide analog should be started prior to transplantation and continued indefinitely post transplant.
Randomized trial comparing monthly ibandronate and weekly alendronate for osteoporosis in patients with primary biliary cirrhosis anxiety disorder symptoms cymbalta 40 mg with mastercard. Raloxifene improves bone mass in osteopenic women with primary biliary cirrhosis: results of a pilot study. Etidronate versus fluoride for treatment of osteopenia in primary biliary cirrhosis: preliminary results after 2 years. An analysis of associated diseases, cardiovascular risk, and malignancies on the basis of mortality figures. Hypercholesterolemia and atherosclerosis in primary biliary cirrhosis: what is the risk Experimental use of pravastatin in patients with primary biliary cirrhosis associated with hypercholesterolemia. Simvastatin in primary biliary cirrhosis: effects on serum lipids and distinct disease markers. Treatment of hypercholesterolemia in patients with primary biliary cirrhosis might be more beneficial than indicated. Primary biliary cirrhosis: survival of a large cohort of symptomatic and asymptomatic patients followed for 24 years. Diagnostic and clinical utility of antibodies against the nuclear body promyelocytic leukaemia and Sp100 antigens in patients with primary biliary cirrhosis. Clinical significance of the fluctuation of primary biliary cirrhosis-related autoantibodies during the course of the disease. Primary biliary cirrhosis has high wait-list mortality among patients listed for liver transplantation. Waiting list mortality of patients with primary biliary cirrhosis in the Japanese transplant allocation system. Transplantation for primary biliary cirrhosis: retrospective analysis of 400 patients in a single center. The effect of liver transplantation on fatigue in patients with primary biliary cirrhosis: a prospective study. Recurrence of primary biliary cirrhosis after liver transplantation: Histologic estimate of incidence and natural history. Primary biliary cirrhosis after liver transplantation: influence of immunosuppression 137. Four year follow up of fatigue in a geographically defined primary biliary cirrhosis patient cohort. Incidence, risk factors, and survival of hepatocellular carcinoma in primary biliary cirrhosis: comparative analysis from two centers. Relatively high risk for hepatocellular carcinoma in patients with primary biliary cirrhosis not responding to ursodeoxycholic acid. Asymptomatic primary biliary cirrhosis: clinical features, prognosis, and symptom progression in a large population based cohort. Epidemiology and natural history of primary biliary cirrhosis in a Canadian health region: a population-based study. The effect of ursodeoxycholic acid therapy on liver fibrosis progression in primary biliary cirrhosis. A multicenter, controlled trial of ursodiol for the treatment of primary biliary cirrhosis. Comparison of the clinical features and clinical course of antimitochondrial antibody-positive and-negative primary biliary cirrhosis. Does antimitochondrial antibody status affect response to treatment in patients with primary biliary cirrhosis Longterm outcomes in antimitochondrial antibody negative primary biliary cirrhosis. Chapter 21: Primary Biliary Cholangitis and human leukocyte antigen locus disparity. Disease recurrence plays a minor role as a cause for retransplantation after living-donor liver transplantation for primary biliary cirrhosis: A multicenter study in Japan. Bile ductal injury and ductular reaction are frequent phenomena with different significance in autoimmune hepatitis. Early stage anxiety symptoms in males discount 30 mg cymbalta with amex, mid stage, and late stage are also acceptable terms, although they sound less scientific. The principal targets of the attack are the bile ducts and the endothelium of veins and arteries but not of sinusoids. These features are variable, and diagnostic findings may or may not present on any individual liver biopsy, so the presence of two of the three features is usually considered sufficient for diagnosis. Cholestasis, hepatocyte ballooning, apoptotic or acidophilic bodies, and focal necrosis may also be present. Chronic (ductopenic) rejection refers to the irreversible damage to the engrafted liver through a combination of immunologically mediated injury and ischemia. It typically follows repeated episodes of acute rejection and so is usually not diagnosed until at least several months after transplantation. Rapidly progressive cases are sometimes seen (acute vanishing bile duct syndrome) but are uncommon. The changes of chronic rejection are thought to be partly due to the injury associated with repeated acute rejection and partly due to reduced arterial flow caused by foam cell arteriopathy in the large arteries of the graft. Bile ducts require an arterial blood supply, so the loss of the arteries contributes to the loss of ducts. Changes of chronic rejection include bile duct atrophy and pyknosis, loss of bile ducts (ductopenia) with or without loss of hepatic artery branches, and foam cell arteriopathy in larger arteries, particularly those near the hilum [73]. The loss of ducts produces features of chronic cholestasis, and zone 3 fibrosis may also occur because of ischemia. Other chronic cholestatic syndromes r Mechanical obstruction: Any of the microscopic changes observed in acute biliary obstruction may be present in biopsy specimens from patients with longstanding obstruction. Additional changes that point to the chronic nature of the process commonly develop when obstruction persists for more than a few weeks. This portal area has several granulomas and considerable fibrosis but lacks a bile duct. Cirrhosis may develop when complete or nearly complete obstruction persists for many months, but most patients will be relieved of the obstruction or will develop complications and death before cirrhosis ensues. Biliary cirrhosis is histologically characterized by fibrous septa, linking portal tracts and outlining irregular islands of parenchyma that resemble the pieces of a jigsaw puzzle. In this condition, all the morphologic features of acute and chronic biliary obstruction described in the preceding text can be observed, depending on the stage during which a biopsy specimen is obtained. The same criteria for the diagnosis of biliary obstruction, described in the preceding text, must be used to differentiate biliary atresia from other cholestatic disorders of the neonate and infant. Some degree of portal fibrosis and ductular proliferation are usually present in biliary atresia and help in distinguishing it from neonatal hepatitis. Diagnostic difficulty may be caused by the presence of giant cell transformation, suggesting hepatocellular injury, in some cases of biliary atresia, but giant cell transformation in neonates should be considered a nonspecific pattern of injury, induced by a variety of hepatic and extrahepatic disorders. In such cases, the liver develops confluent granulomas that destroy bile ducts, cause chronic cholestasis, and may lead to biliary cirrhosis. Although depletion of bile ducts is characteristic, florid duct lesions are uncommon. Secondary sclerosing cholangitis may also follow chemical injury, such as intra-arterial Chapter 6: Hepatic Histopathology 165 acinar ("interlobular") ducts [79]. Bile ducts are present at birth but undergo progressive destruction from early infancy to childhood. Despite the lack of ducts, it is rare to see bile stasis, and progressive fibrosis or cirrhosis is uncommon. By contrast, children who have bile duct paucity without the other anomalies of Alagille syndrome tend to have a much worse disease, often with progression to end-stage liver disease. Such cases are usually idiopathic but are thought to result from various types of in utero injuries that prevent the normal development of acinar ducts, resulting in a diminished number of ducts at birth. The distinction is not always sharp, and there are cases where both macrovesicular and microvesicular fat coexist. Order cymbalta in india. HyCosy Test Anxiety & Results! | TTC After Ectopic Pregnancy.
|