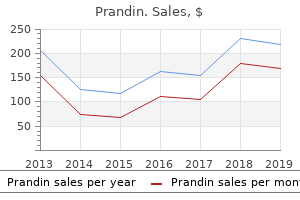
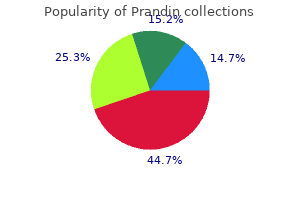
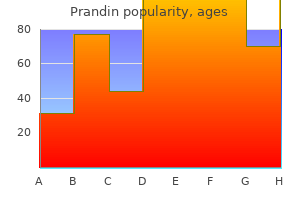
Prandin"Generic prandin 1 mg free shipping, diabetic ulcer grading". By: Q. Giores, M.B.A., M.B.B.S., M.H.S. Clinical Director, Louisiana State University School of Medicine in New Orleans These extensive neuroglial cells form much of the total retinal volume and almost totally fill the extracellular space between neural elements diabetes test machines best 2mg prandin with amex. The cell bodies of retinal astrocytes lie between the layer of nerve fibres and the internal limiting membrane, while their processes branch to form sheaths around ganglion cell axons. They are present only in regions of the retina that are vascularized and are therefore absent from the fovea. Astrocytes contribute substantially to the glia limitans, which surrounds the capillaries. Their radiating branched processes spread mainly parallel to the retinal plane, and this gives them a star-like appearance when viewed microscopically from the surface of the retina. The expanded end-feet of radial glial cells and astrocytes are separated from the vitreous body by a complex, rather thick (0. The delicate collagen fibrils of the vitreous body blend with the glial basal lamina. The internal limiting membrane is involved in fluid exchange between the vitreous and the retina and, perhaps through the latter, with the choroid. It has various other functions, including anchorage of retinal glial cells and inhibition of cell migration into the vitreous body. Optic Disc and Retinal Blood Vessels the retina is placed between two sets of arteries and veins-the ciliary vessels of the choroid, and the branches of the central retinal vessels. It depends on both circulations because neither is sufficient by itself to maintain full visual activity in the retina. The central retinal vessels enter and leave the retina at the optic disc, which is described first; then the vessels are considered. It is the exit point for the optic nerve fibres and a point of entry and exit for the retinal circulation. It is the only site where anastomoses occur with other arteries (the posterior ciliary arteries). It is visible, by ophthalmoscopy, and is a region of much clinical importance; it is here that the central vessels can be inspected directly-the only vessels so accessible in the whole body. Oedema of the disc (papilloedema) may be the first sign of raised intracranial pressure, which is transmitted into the subarachnoid space around the optic nerve and compresses the central retinal vein where it crosses the space. The optic disc is superomedial to the posterior pole of the eye, so it lies away from the visual axis. In light-skinned subjects, the general retinal hue is a bright terra-cotta red, with which the pale pink of the disc contrasts sharply; its central part is usually even paler and may be light grey. These differences are due in part to the degree of vascularization of the two regions, which is much less at the optic disc; it is also due to the total absence of choroidal or retinal pigment cells, because the retina is represented in the disc by little more than the internal limiting membrane. The optic disc does not project at all in many eyes, and rarely does it project sufficiently to justify the term papilla. It is usually a little elevated on its lateral side, where the papillomacular nerve fibres turn into the optic nerve. There is usually a slight depression where the retinal vessels traverse its centre. The central retinal artery enters the optic nerve as a branch of the ophthalmic artery, approximately 1. It travels in the optic nerve to its head, where its fascicles traverse the lamina cribrosa. At this level, which is usually not visible with ophthalmoscopy, the central artery divides into two equal branches, superior and inferior. After a few millimetres, these divide into superior and inferior nasal branches and superior and inferior temporal branches. However, the courses of the venous and arterial vessels do not correspond exactly, and arteries often cross veins, usually lying superficial to them. In severe hypertension, the arteries may press on the veins and cause visible dilatation distal to these crossings.
Respiratory support in an intensive care unit is essential if the vital capacity is less than 1 litre diabetic meters purchase prandin without prescription. Steroids, immunosuppression, intravenous gammaglobulin and plasma exchange have all been shown to be effective treatment. Plasmapheresis or intravenous gamma globulin shortens the time to recovery from respiratory paralysis and hastens the return of mobility. Rapid improvement is much more likely if treatment is begun within 2 weeks of the first symptoms. Relapses may occur and are more common after intravenous gamma globulin than after plasmapheresis. The differential diagnosis of acute ascending motor paralysis includes diphtheria, polio, polyarteritis nodosa, acute intermittent porphyria, tick or snake bites and rhabdomyolysis, arsenic poisoning and botulism. Remember that diphtheria, botulism and myasthenia gravis usually begin with bulbar symptoms. The differential diagnosis of autonomic neuropathy includes diabetes mellitus, alcoholism, acute intermittent porphyria and amyloidosis. A careful history and physical examination should enable the candidate to produce a sensible differential diagnosis and management plan. Causes of this condition can include cardiac arrhythmias, postural hypotension, cough syncope and micturition syncope. Vasovagal syncope or presyncope can often be diagnosed clinically if the history is typical: an episode begins with clamminess, sweating and nausea and often occurs in a crowded room or after something upsetting has happened. Generalised epilepsy may be associated with myoclonic jerks (juvenile myoclonic epilepsy), but frequently occurs with sudden loss of consciousness without warning. Eyewitnesses are likely to find a seizure more frightening than a syncopal episode. Idiopathic generalised epilepsy is frequently symmetrical with tonic (stiffening) and then clonic (brief jerking movements) phases, whereas partial seizures with secondary generalisation may be associated with asymmetric posturing initially. Presyncope refers to a sense of impending loss of consciousness, manifest as faintness or light-headedness, and is often associated with sweating, nausea, anxiety and visual dimming. Complex partial seizures involve altered consciousness when the seizure spreads to involve one or both temporal lobes. Patients may stare and not respond, and may posture, turn their head or perform automatic motor tasks c. Secondarily generalised seizures cause convulsions and occur when a partial seizure spreads to involve both hemispheres diffusely. These convulsions involve impaired awareness followed by generalised muscle contractions (tonic) and then rhythmical contraction and relaxation of muscles (clonic) movements. They may be hard to distinguish from primary generalised seizures, but sometimes focal features such as asymmetric posturing or the report of a preceding aura help to make the diagnosis. Jacksonian seizures are simple motor seizures characterised by rhythmical contraction of a group of muscles (typically of the fingers) that spread to the arm and then the ipsilateral side of the face. Partial seizures may be preceded by an aura, particularly if the seizure activity begins in the temporal lobe. Primary generalised tonic and clonic seizures are convulsions that may occur with no warning. Tongue biting and incontinence are common, and a feeling of confusion and tiredness is common afterwards b. Absence seizures are generalised seizures that cause momentary loss of consciousness. Myoclonic seizures are very brief jerky movements that occur without warning, often when the patient is tired or in the morning. If epilepsy has been diagnosed or is suspected, ask the patient how this has been discussed and what restrictions have been placed on his or her activities. Cerebellar stroke characteristically causes severe associated nausea and vomiting, and is of sudden onset. Unsteadiness of gait may be secondary to a number of disorders of the peripheral or central nervous system.
Minimizing the number of pleural punctures reduces the risk of procedure-related pneumothorax diabetic lifestyle cheap 0.5 mg prandin overnight delivery. A halo (> 5 mm) completely encircling the nodule is a predictor of treatment success. The mass is in close proximity to both the ascending and descending thoracic aorta. The pulmonary arteries course below the mass, and the transverse portion of the thoracic aortic arch is immediately adjacent. The abnormality was felt to represent either an aneurysmal bone cyst or a giant cell tumor. This expansile mass has shell-like calcifications and an associated destructive process involving the contiguous thoracic vertebral body, pedicle, and right transverse process. A prominent vascular pedicle arising from the suprarenal abdominal aorta courses toward the mass. Selective catheterization of the right internal mammary artery shows extensive tumor vascularity. This was embolized with a Gelfoam slurry using the same coaxial technique that was employed in the right internal mammary artery. There is no filling of either the distal internal mammary or inferior phrenic arteries. Embolization: Benign Lung Mass (Gross Pathology Specimen) Embolization: Benign Lung Mass (Gross Pathology Specimen) (Left) After embolization the mass was successfully resected in its entirety, with minimal blood loss. Gross pathology specimen shows the well-encapsulated solitary fibrous tumor, which is a rare mesenchymal tumor that typically arises from the visceral pleura & is often quite large. Embolization: Benign Lung Mass (Microscopic Pathology Specimen) Embolization: Benign Lung Mass (Postoperative Chest Radiograph) (Left) Microscopic pathology section from the resected solitary fibrous tumor shows thrombosed vascular channels that contain Gelfoam particles from the transcatheter embolization. The mediastinal structures have resumed a midline position, and there is no evidence of any residual mass. Cryoablation: Bladder Cancer Metastasis Arteriovenous Shunting: Renal Cell Carcinoma Metastasis (Arterial Phase) (Left) A superficial femoral artery angiogram shows enlarged arterial branches supplying a hypervascular, lytic destructive metastasis invading the distal femur. This has implications for the choice of embolic agent used to treat the lesion due to the high risk of nontarget embolization from the embolic agent shunting through the fistula. Clinically, patients with osteoid osteoma experience pain that is worse at night and may be relieved with nonsteroidal antiinflammatory drugs. Because the symptomatology may last for many years, percutaneous ablation is a valuable and effective treatment option. Ablation: Osteoid Osteoma (Biopsy Prior to Ablation) Ablation: Osteoid Osteoma (Radiofrequency Probe in Position) (Left) A hand drill has been bored through the tibia until the tip is within 1 mm of the anterior margin of the nidus. After removing the drill from the cannula, a biopsy needle is advanced into the nidus and a specimen obtained. The probe and grounding pads are connected to the generator, and the automatic ablation program is activated. In this case, an anterior approach was used in order to avoid the posterior neurovascular structures. Embolization: Thyroid Carcinoma Metastasis (Posterior Circumflex Particle Embolization) Embolization: Thyroid Carcinoma Metastasis (Anterior Circumflex Particle Embolization) (Left) A microcatheter was introduced coaxially via the 5Fr catheter in the axillary artery into the posterior circumflex humeral artery. Embolization with 300- to 500-m particles was performed with marked reduction of the tumor vascularity. Intraoperative hemostasis was excellent due to the transcatheter tumor embolization. The anterior temporal branch remains patent and is again seen arising from the mid M1 segment. Berlin Heidelberg: Springer-Verlag, 2006 Hacke W et al: Intravenous thrombolysis with recombinant tissue plasminogen activator for acute hemispheric stroke. The device was only slightly recaptured prior to removal to prevent dislodging this thrombus. Rosenfield K et al: Randomized trial of stent versus surgery for asymptomatic carotid stenosis. Carotid Artery Stent Procedure (Angioplasty Prior to Stenting) Carotid Artery Stent Procedure (Stent Position Before Deployment) (Left) Lateral intraoperative fluoroscopic spot image shows a 2. Discount prandin 2mg visa. मधुमेह से मुख्ती | How to Reverse & Cure Diabetes Permanently | Dr.Education (Hindi). Stents are reserved for complications of balloon angioplasty diabetes foot pain purchase prandin with paypal, such as flow limiting dissection or vessel rupture. Both stents project into aortic lumen by 1-2 mm, which is considered to be ideal positioning. Treatment of bilateral stenoses in one setting may be performed if contrast volume is kept low. Renal Artery Stenosis (Post Treatment Angiogram) Ostial Atherosclerotic Stenosis (Treatment With Angioplasty) (Left) Graphic shows that balloon angioplasty of an ostial atherosclerotic stenosis is often ineffective, as the plaques will recoil upon deflation and removal of the angioplasty balloon. This graphic shows a balloonmounted stent correctly placed at the site of the stenosis, projecting 1-2 mm into the aortic lumen. This position prevents the aortic plaque from covering the proximal portion of the stent and prevents plaque recoil. The stenosis and irregularity is better defined by the selective renal arteriogram. An angled sheath, such as an Ansel sheath, is then advanced over the wire an into the renal ostium. Repeat angiogram through the sheath can be performed to confirm desired location of the stent. Mild residual irregularity of the artery is expected after angioplasty: Avoid the urge to over dilate or stent. Fibromuscular Dysplasia (Balloon Dilation) Fibromuscular Dysplasia (Postprocedure Angiogram) (Left) Because of her severe hypertension, despite the mild angiographic appearance, it was decided to proceed with balloon angioplasty. After a wire was used to traverse the lesion, a 6-Fr Ansel sheath was advanced into the renal artery ostium. The guidewire was kept in place until confirmation of procedural success and exclusion of significant complications. This can lead to arterial thrombosis and irreversible renal ischemia if not treated promptly. Treatment options for an in-stent stenosis include restenting with a covered stent or balloon angioplasty. A guidewire has been passed through the stenotic lesion, and the tip has been positioned distally. The balloon used was inappropriately sized, chosen to match the size of the adjacent aneurysm. A selective right renal angiogram through this sheath showed severe ostial stenosis. Pressures were measured across the stenosis with an initial gradient of 52 mm Hg Renal Artery Stent Fracture (Selective Renal Angiogram Through Sheath) 426 Renal Arteries: Revascularization Arterial Procedures Renal Artery Stent Fracture (Post 1st Stent Placement Angiogram) Renal Artery Stent Fracture (Final Angiogram) (Left) A 6x15-mm PalMaz Blue balloon expandable stent was chosen. Spot radiography at the time of her repeat angiogram showed an unexpected finding, a fracture of the superior portion of the stent. A 7-mm balloon was advanced and, through repeated gentle back and forth movements, the fracture was intentionally completed. Renal Artery Stent Fracture (Treatment of Fracture Stent) Renal Artery Fracture (Final Renal Angiogram) (Left) (A) the fractured portion of the stent was then deployed in the left iliac artery, using an 8-mm balloon. Markedly elevated peak systolic velocity (240 cm/second) and aliasing at the origin of the transplanted renal artery are consistent with stenosis at the external iliac to transplanted renal artery anastomosis. Transplant Renal Artery Stenosis Transplant Renal Artery Stenosis (Left) Given the worsening renal function, the decision was made to proceed with angiogram and possible intervention. Angiography confirmed severe stenosis at the origin of the transplanted renal artery. Transplant Renal Artery Stenosis (Stent Migration) Transplant Renal Artery Stenosis (Stent Migration) (Left) Repeat angiogram prior to deployment of the balloon expandable stent shows it is positioned well, extending slightly into the external iliac artery beyond the ostium of the renal artery. This malpositioning precludes subsequent renal artery intervention and places the iliac artery at risk for subsequent stenosis. When considering revascularization of an acutely ischemic kidney, the previously thought 1- to 3hour window for revascularization is too short, as positive outcomes have been reported with initiation of the procedure up to 19 hours after the ischemic event. Angiogram showed occlusion of the mid right renal artery with a meniscus of contrast at the proximal portion of the clot and focal expansion of the occluded portion of the renal artery. The goal is to devascularize the tumor while preserving adjacent normal renal parenchyma. Hellmund A et al: Rupture of renal artery aneurysm during late pregnancy: clinical features and diagnosis.
|