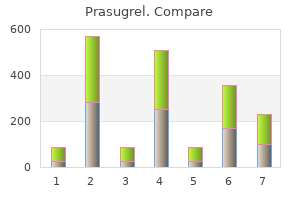
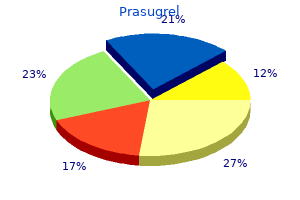
Prasugrel"Discount prasugrel online amex, medications janumet". By: Q. Lester, M.A., Ph.D. Clinical Director, Florida Atlantic University Charles E. Schmidt College of Medicine Although patients with status epilepticus may have poorer response to drug treatment medicine information 10 mg prasugrel, at least among children [32,33], those who become seizure-free do not seem to have a higher risk of relapse. Influence of individual drugs It is often suggested that the risk of seizure recurrence differs depending on the drug that is to be withdrawn. Withdrawal seizures are particularly said to occur with the discontinuation of benzodiazepines and phenobarbital. The temporal pattern of seizure recurrence was similar in the barbiturate group and the other groups. Perhaps surprisingly, the withdrawal of carbamazepine was associated with a lower relative risk of seizure recurrence on withdrawal than were other drugs even after adjustment for other predictors of outcome [34]. The clinical usefulness of such models remains uncertain because they have not been prospectively validated in external cohorts. Antiepileptic drug withdrawal after epilepsy surgery Compared with the large body of literature on treatment withdrawal in patients treated medically, there is a dearth of information about the pharmacological management in postsurgical seizure-free patients. There has been no randomized controlled trial to examine these issues, and only few studies have reported clinical experience from individual centres in patients undergoing a mixture of surgical procedures. Other recent retrospective uncontrolled studies in adults [40,41,42] and children [43] have not shown substantially different findings. Physical consequences of seizure relapse may entail accidental injuries, burns, fractures or even death. Of these, one died only a few weeks after withdrawal and one died 4 years after withdrawal [8]. Seizure relapse may have social consequences such as impact on employment and driving. In many countries, not having had a daytime seizure for a certain length of time will qualify for reinstatement of a driving licence, and seizure relapse may lead to loss of this privilege. Seizure control after relapse Evidence from previous studies showed the majority of patients who relapse after medication is stopped will regain acceptable control when treatment is reintroduced. The differences between these studies may have arisen from the methodological differences in inclusion of patients, length of follow-up and the definition of remission. Factors associated with a poorer outcome after relapse were the occurrence of a partial seizure at the time of relapse, a previous history of seizures while on medication and shorter duration of seizure freedom prior to the relapse [48]. Withdrawal may lead to cessation of adverse effects that the patient is experiencing at present, particularly neurocognitive side-effects, as well as avoidance of complications associated with long-term use. For some patients, the responsibility of remembering to take medication on time and obtaining repeat prescriptions is an unwanted source of stress. For many patients, continued therapy, with or without seizures, implies continued epilepsy. However, measuring these improvements may be logistically difficult from a research standpoint. The authors suggested that the double-blinded design of the study excluded one known positive effect of being off medication, namely not having to take drugs regularly, and that fear of seizure relapse due to patients being blinded might even have had a negative impact on quality of life. Both enzyme- and non-enzyme-inducing agents have been implicated, albeit it on relatively weak evidence, and their effects may be additive and progressive with duration of treatment [52]. Although evidence is conflicting, long-term treatment with valproate may be associated with various endocrine abnormalities including polycystic ovarian syndrome [53]. These issues demand careful consideration and discussion, and ultimately the decision can only be made by the patient. For example, a 25-year-old man whose job is dependent on holding a driving licence might well feel that a 40% risk of seizure recurrence on drug withdrawal is unacceptable. However, a similar risk in his 25-year-old wife might be acceptable if it allowed a drug-free pregnancy. This number was considerably reduced (to 9%) by the use of a predictive model, which presented the risk of seizure recurrence for policies of continued treatment and withdrawal. The latter policy consistently predicted greater risks of relapse than did the former. Only 10% of subjects (almost entirely adults) decided to withdraw treatment after reviewing the results of the model. Treating repetitive seizures with a rectal diazepam formulation: a randomized study medicine synonym cheap 10 mg prasugrel mastercard. Buccal midazolam and rectal diazepam for treatment of prolonged seizures in childhood and adolescence: a randomised trial [see comments]. Safety and efficacy of buccal midazolam versus rectal diazepam for emergency treatment of seizures in children: a randomised controlled trial. Midazolam versus diazepam for the treatment of status epilepticus in children and young adults: a meta-analysis. A randomized controlled trial of intranasal-midazolam versus intravenous-diazepam for acute childhood seizures. Intranasal versus intravenous lorazepam for control of acute seizures in children: a randomized open-label study. A prospective, randomized study comparing intramuscular midazolam with intravenous diazepam for the treatment of seizures in children. Status epilepticus: divergence of sympathetic activity and cardiovascular response. Systemic factors and epileptic brain damage: prolonged seizures in paralyzed, artificially ventilated baboons. Prolonged epileptic seizures in primates: ischemic cell change and its relation to ictal physiological events. Metabolic abnormalities and new-onset seizures in human immunodeficiency virus-seropositive patients. The relative effectiveness of five antiepileptic drugs in treatment of benzodiazepine-resistant convulsive status epilepticus: a meta-analysis of published studies. Pharmacokinetics and clinical effect of phenobarbital in children with severe falciparum malaria and convulsions. Efficacy and safety of intravenous sodium valproate versus phenobarbital in controlling convulsive status epilepticus and acute prolonged convulsive seizures in children: a randomised trial. A case of Angelman syndrome representing with myoclonic status successfully treated with phenobarbital. Pharmacokinetics and clinical effects of phenytoin and fosphenytoin in children with severe malaria and status epilepticus. Reassessment of phenytoin for treatment of late stage progressive myoclonus epilepsy complicated with status epilepticus. Clinical and pharmacological approaches of status epilepticus in children: personal experience. Predictors and prognosis of status epilepticus treated with intravenous sodium valproate. Efficacy of intravenous levetiracetam as an add-on treatment in status epilepticus: a multicentric observational study. Safety and efficacy of intravenous valproate in pediatric status epilepticus and acute repetitive seizures. Intravenous valproate associated with significant hypotension in the treatment of status epilepticus. Valproate is an effective, well-tolerated drug for treatment of status epilepticus/serial attacks in adults. Intravenous valproate for seizures in 137 Taiwanese children: valproate naive and non-naive. Intravenous sodium valproate in mainland China for the treatment of diazepam refractory convulsive status epilepticus. Efficacy and safety of intravenous valproate for status epilepticus: a systematic review. Super-refractory status epilepticus: an approach to therapy in this difficult clinical situation. Barbiturate anesthesia in the treatment of status epilepticus: clinical experience with 14 patients. Electroencephalographic criteria for nonconvulsive status epilepticus: synopsis and comprehensive survey. Autistic regression and disintegrative disorder: how important the role of epilepsy Persistent nonconvulsive status epilepticus after the control of convulsive status epilepticus. Discount prasugrel 10mg with amex. My health conditions: Life with Long QT Syndrome..
Surgical debridement should be employed treatment ear infection order prasugrel with mastercard, if appropriate (as in postneurosurgical infections and brain abscess). Supportive care, consisting of hydration, electrolyte replacement, antipyretics, antiemetics, analgesics, antiepileptic drugs, and wound care (for surgical wounds), is an important adjunct to antimicrobial therapy, particularly early in the treatment course. Although there are no prospective studies that relate timing of antibiotic administration to clinical outcome in bacterial meningitis, a longer duration of symptoms and more advanced disease before treatment initiation increase the risk of a poor outcome. Ability of antibiotics to reach and achieve effective concentrations at the infection site is the key to treatment success. Prompt recognition and diagnosis are essential so that antimicrobial therapy can be initiated as quickly as possible. A medical history (including risk factors for infection and history of possible recent exposures) and physical examination yield important information to help guide the diagnosis and treatment of meningitis. Common signs and symptoms include fever, headache, nuchal rigidity (stiff neck), and photophobia. Infants present with nonspecific signs and symptoms, including excessive irritability or crying, vomiting or diarrhea, tachypnea, altered sleep pattern, and poor eating. Depending on involved pathogens and disease severity, patients may also present with altered mental status, stupor, and seizures. As her friends at the home learn of her illness, they are concerned about the possibility of getting sick and begin to follow up with the on-call physician at the group home. What oral options are viable options for continuation as an outpatient in this case Empirical treatment regimens now include the combination of a third-generation cephalosporin plus vancomycin. Carefully selected patients who have close medical monitoring and follow-up may be able to receive a portion of their parenteral meningitis treatment on an outpatient basis. Pathogen-Directed Antimicrobial Therapy Empirical antimicrobial therapy should be modified on the basis of laboratory data and clinical response. From 11% to 19% of survivors of meningococcal meningitis experience long-term sequelae, including hearing loss, limb loss, and neurologic deficits. In the United States, serotypes B, C, and Y each are responsible for approximately 30% of cases. Infants younger than 1 year are at highest risk, possibly because pneumococcal vaccination reduces bactericidal antibodies. Meningococcal disease is often (approximately 50%) associated with a diffuse petechial rash, and patients may experience behavioral changes. Patients may develop fulminant meningococcal sepsis, characterized by shock, disseminated intravascular coagulation, and multiorgan failure. Treatment should be continued for 7 days, after which no further treatment is necessary. Prevention of meningococcal disease by vaccination is a key to reducing the incidence of meningococcal meningitis. Routine vaccination should be administered between ages 11 and 21 years (preferably as soon as possible), with quadrivalent vaccine that provides protection against serogroups A, C, Y, and W. The quadrivalent conjugate meningococcal vaccine protects against four of the five serotypes causing invasive disease (A, C, Y, and W-135). Meningococcal vaccines do not protect against serotype B, which causes more than 50% of the cases of meningococcal meningitis in children younger than 2 years. Patients with a history of type I penicillin or cephalosporin allergy may be treated with vancomycin. Treatment should be continued for 10 to 14 days, after which no further maintenance therapy is required. Administration of vaccines to high-risk individuals is a key strategy to reduce the risk of invasive pneumococcal disease. However, 2013 reports note only 82% of children aged 35 months completed the full series of the pneumococcal conjugate vaccine.
Deferasirox should be initiated at 20 mg/kg daily and is available in a tablet that should be dispersed in water medicine lookup cheap prasugrel uk, orange juice, or apple juice and taken orally 30 minutes before food. Due to alloimmunization, an acute or delayed transfusion reaction may occur 5 to 20 days posttransfusion. Patients may develop symptoms suggestive of a pain crisis or worsening symptoms if they are already in crisis. Transfusions also may be useful in patients with complicated obstetric problems, refractory leg ulcers, refractory and prolonged pain crises, or severe priapism. Volume overload leading to congestive heart failure is more likely to occur if the anemia is corrected too rapidly in patients with severe anemia and should be avoided. If staphylococcal infection is suspected due to previous history or the patient appears acutely ill, vancomycin should be initiated. While the patient is receiving broad-spectrum antibiotics, their regular use of penicillin for prophylaxis can be suspended. Because of the risk of dehydration during infection with fever, increased fluid may be needed. Cerebrovascular Accidents Acute neurologic events, such as stroke, will require hospitalization and close monitoring. Patients with a history of seizure may need anticonvulsants, and interventions for increased intracranial pressure should be initiated if necessary. Children with history of stroke should be initiated on chronic transfusion therapy. Incentive spirometry helps the patient take long, slow breaths to increase lung expansion. Appropriate management of pain is important, but analgesic-induced hypoventilation should be avoided. Patients should maintain appropriate fluid balance because overhydration can lead to pulmonary edema and respiratory distress. Oxygen therapy should be utilized in any patient presenting with respiratory distress or hypoxia. Stuttering priapism, where erection episodes last anywhere from a few minutes to less than 2 hours, resolves spontaneously. Goals of therapy are to provide pain relief, reduce anxiety, provide detumescence, and preserve testicular function and fertility. Vasoconstrictors are thought to work by forcing blood out of the cavernosum and into the venous return. Pseudoephedrine dosed at 30 to 60 mg daily taken at bedtime has been used to prevent or decrease the number of episodes of priapism. Pregnant individuals should avoid contact with infected patients because midtrimester infection with parvovirus may cause hydrops fetalis and still birth. Splenectomy is usually delayed until after 2 years of age to lessen the risk of postsplenectomy septicemia. Patients with mild pain crisis may be treated as outpatients with rest, warm compresses to the affected (painful) area, increased fluid intake, and oral analgesia. Infection should be ruled out because it may trigger a pain crisis, and any patient presenting with fever or critical illness should be started on empirical broad-spectrum antibiotics. Assess pain on a regular basis (every 2 to 4 hours), and individualize management to the patient. Obtain a good medication history of what has worked well for the patient in the past. Monitor for the total amount of acetaminophen given daily, because many products contain acetaminophen. Maximum daily dose of acetaminophen for adults is 4 g/day, and for children, five doses over a 24-hour period.
|