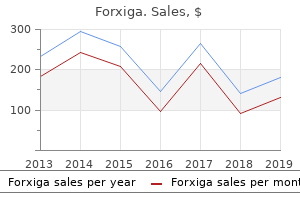
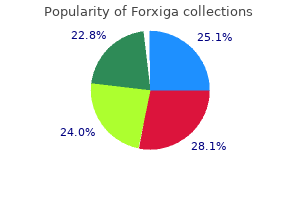
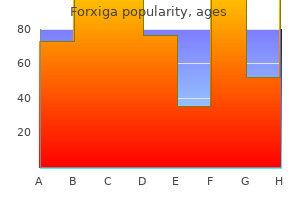
Forxiga"Generic forxiga 5mg amex, diabetes prevention and control program". By: H. Uruk, MD Clinical Director, Rutgers New Jersey Medical School Age the mean age of onset of symptoms in mixed cryoglobulinaemia is reported as being 53 years diabetic diet 2000 calories order forxiga with paypal, with a mean age at diagnosis of 56 years [3]. Pathophysiology Type I cryoglobulins are single monoclonal immunoglobulins usually associated with haematological disorders, such as multiple myeloma, macroglobulinaemia and lymphoma. Mixed cryoglobulinaemia causes a systemic vasculitis with multiorgan involvement, mainly of the skin, joints, kidneys and peripheral nerves. In cryoglobulinaemia of all types, other skin signs are livedo reticularis, Raynaud phenomenon, atypical ulceration of the legs, digital skin necrosis and cold urticaria [6]. Differential diagnosis Other causes of vascular occlusion such as hypercoagulable states, embolic disease and vasculitides need to be included in the differential diagnosis. If cryoglobulinaemic vasculitis is suspected clinically, investigations should demonstrate circulating cryoglobulins, high rheumatoid factor titre and low C4 levels. Histology may show a leukocytoclastic vasculitis of the small blood vessels on a skin biopsy. Histopathology of cryoglobulinaemia without vasculitis will reveal homogeneous eosinophilic material within the vascular lumina of dermal vessels, which corresponds to cryoglobulin deposits. Management Treatment of mixed cryoglobulinaemia is aimed at reducing immune complex activity by immunosuppression (with prednisolone and cyclophosphamide) and plasmapheresis. Energy is inversely proportional to wavelength, therefore most biological effects are seen at shorter wavelengths. Experimental effects Acute effects Infrared radiation alone produces erythema, which disappears by 6 h [4]. Cold agglutinins t Cold agglutinin disease is a disorder of autoimmune haemolysis in which coldsensitive immunoglobulins react against erythrocyte surface antigens. Cutaneous features occur mainly on acral sites and include Raynaud phenomenon, acrocyanosis and skin necrosis. The results of therapy with corticosteroids, alkylating agents and interferon have been poor. Sources other than domestic heating may be responsible for erythema ab igne at other body sites. Examples include the repeated application of hot water bottles or heated pads for chronic backache, recliner chairs with builtin heaters [2] and even bathing in hot water [3]. Among occupations, foundry workers and bakers and the various tasks that involve carrying heated coals are sometimes relevant. It has been reported as a useful marker of chronic pancreatitis because local heat relieves the abdominal pain [9] but also occurs when heat is applied for other real and imagined pains [10], including cancer [11]. In mentally disturbed patients with thermophilia, bizarre areas of erythema ab igne are sometimes encountered. Pathophysiology Pathology In the early stages, epidermal atrophy, dermal pigmentation and vasodilatation are evident. Basophilic degeneration of the connective tissue, focal hyperkeratosis and epithelial cellular atypia occur later, closely resembling the changes induced by actinic damage [12]. Electron microscopy shows similar changes in the elastic fibres as found in chronic sun exposure [13]. Further or repeated exposure causes a more marked erythema with noticeable hyperpigmentation and, sometimes, superficial epidermal atrophy. The cumulative effects of the small and repeated thermal exposures often clear during the summer months but involution gradually becomes less complete. The distribution of the dermatosis depends not only on the direction of the incident radiation, but also on the contour of the skin and the interposition of clothing. When erythema ab igne results from sitting in front of the fire, people may sit sideways, causing the outer aspect of one leg and the inner aspect of the other to be particularly affected. Others habitually sit directly in front, and a strictly symmetrical eruption is seen. In severely affected individuals the reticular pattern is lost, a wide area of skin becoming pigmented and atrophic, with only the periphery showing the characteristic pattern. An unusual variant has been described in elderly immobile females with lymphoedema in which there are reticulate ridges of tissue that can be compressed [21]. Rarely, lichen planus, psoriasis or chilblain lupus may appear as a Koebner phenomenon in the affected area.
Dermatological diseases Several dermatoses can be associated with oral ulcers or erosions; lichen planus is the most common diabetes high blood pressure buy cheap forxiga 10mg online, pemphigus the most serious and pemphgoid is intermediate. Dermatitis herpetiformis and adult linear IgA disease (see Chapter 50) Oral lesions may occur in dermatitis herpetiformis and in most patients with linear IgA disease. These disorders must be differentiated, especially from pemphigoid, angina bullosa haemorrhagica, superficial mucocoeles and lichen planus. Salivary IgA antigliadin antibodies may be found but this is not useful diagnostically. Dapsone and sulfapyridine are the most effective therapeutic agents along with a glutenfree diet in dermatitis herpetiformis. Mycophenolate mofetil may be of benefit in the treatment of linear IgA disease [13]. Biopsy of perilesional tissue with immunostaining and histological examination may help, although pathology can be variable and immunostaining is not specific. No specific treatment is available but supportive care is important; a liquid diet and intravenous fluid therapy may be necessary. Levamisole [22,23] and thalidomide have occasionally been used to some effect [24,25]. Continuous therapy with valaciclovir 500 mg twice a day has also been reported to be effective [1,2,10,27]. The pathology is similar to that of cutaneous lichen planus, although sawtooth rete ridges are rarely seen in oral biopsies, and other epithelial changes may be less distinct. The common oral lesions of lichen planus are bilateral white lesions in the buccal and/or lingual mucosa. Most oral lichen planus is idiopathic but significantly greater anxiety and depression are observed among patients with oral lichen planus compared with controls [8,9]. The surrounding mucosa is often erythematous and glazed in appearance, with loss of filiform papillae of the tongue, and there are often pathognomonic whitish striae. Biopsy with immunofluorescence is often indicated to exclude keratosis, chronic ulcerative stomatitis with stratified epitheliumspecific antinuclear antibodies, lichen sclerosus, lupus erythematosus, malignancy and other disorders. It may be wise to consider removal of dental amalgams if the lesions are closely related to these, or are unilateral [22], but there are no tests. There is no evidence that either lichen planus or lichenoid lesions patients would routinely benefit from having all their amalgam restorations replaced. Weak evidence from potentially very biased, small nonrandomized unblinded studies suggests that a small fraction of patients may benefit from targeted amalgam replacement. Topical aloe vera, topical pimecrolimus and oral curcuminoids are the most promising new treatment modalities. Other interesting topical modalities are topically applied thalidomide and amlexanox.
Oral submucous fibrosis: an overview of the aetiology diabetes insipidus peds in review buy forxiga 10 mg online, pathogenesis, classification, and principles of management. Potentially malignant disorders of the oral cavity: Current practice and future directions in the clinic and laboratory. Oral soreness without ulceration Burning mouth syndrome 22 Buchanan J, Zakrzewska J. Pemphigus vulgaris: update on etiopathogenesis, oral manifestations and management. Acquired lip lesions Actinic cheilitis 1 Markopoulos A, AlbanidouFarmaki E, Kayavis I. Actinic prurigo cheilitis: clinicopathologic analysis and therapeutic results in 116 cases. Characterization and management of exfoliative cheilitis: a singlecenter experience. Cheilitis granulomatosa: overview of 13 patients with longterm followupresults of management. Angina bullosa haemorrhagica: presentation of eight new cases and a review of the literature. Desquamative gingivitis; retrospective analysis of disease associations of a large cohort. Careful dermatological evaluation, including a full history and complete examination, usually allows confident clinical differen tial diagnosis. It is important to consider the possibility of sexually transmitted disease or a urological disorder and refer accordingly; combined clinics are useful. Itching, rashes and tumours are the major components of gen eral dermatology and the genitocrural area is not spared. Itch occurring in the absence of specific diagnostic skin lesions is not usually confined to the genitocrural area, but if so it should not be labelled as psychogenic until all pos sible causes have been excluded. The intensity with which itch can be perceived in the anogenital area may be a result of the vagaries of cortical representation afforded the region in the sensorium as well as anxiety about exposure to sexually transmitted disease and genital cleanliness. Complete examination is mandatory to elicit important signs at extragenital sites. The physical examination of the male at any age is incomplete without examination of the genitals and scrotum (but this is frequently not carried out in general clinical settings) Box 111. The presence or absence of the prepuce, phimosis or paraphimosis should be sought and the foreskin retracted gently (if present). Findings specific to the male genitalia include phimosis, para phimosis, balanitis and posthitis. In adults, phi mosis is usually the consequence of a number of disease processes, including titanium balanitis attributed to titanium formulated in proprietary topical preparations [4]. In boys, the histo logical findings may be normal in nearly half of those circumcised [6]. This finding does not exclude lichen sclerosus or other der matoses, since the prepuce may not be the seat of the disease, but might contribute to it. Rickwood [8] has said that paraphimosis results from abuse not disease of the foreskin, but some medical causes can be identified (Box 111. Balanitis is inflammation of the glans penis; posthitis is inflam mation of the prepuce [9]. Balanoposthitis means inflammation of the glans and prepuce, and can be regarded as a special form of intertrigo (Boxes 111. Generally, dermatologists feel that balani tis, posthitis and balanoposthitis are probably more commonly caused by inflammatory and precancerous dermatoses than do genitourinary physicians, who teach that most cases are caused by infection, usually with Candida [10,11]. However, the evidence for Candida as a primary cause of balanoposthitis is not strong [12]. The principal causes of male genital ulceration are sexually trans mitted and nonsexually transmitted infection, cancer and artefact [13]. Dor sal perforation of the prepuce is a recently highlighted complica tion of several ulcerative penile diseases, sexually and nonsexually acquired, as listed in Box 111. Penile necrosis is a rare but devastating presentation with an important differential diagnosis. A penis biopsy is not often necessary but can be informative in carefully selected cases of suspected neo plasia rather than the differential diagnosis of the inflammatory dermatoses [21,22].
Other histological features are elongated dermal papillae blood glucose test kit forxiga 5mg with visa, acanthosis, a prominent granular layer often containing koilocytes, and a stratum corneum of variable thickness. Management Treatment of genital warts is usually undertaken in the setting of a genitourinary clinic. The new immune response modulating cream, imiquimod, is now used for resistant cases or patients with extensive lesions. This has to be used with care as it also induces an inflammatory response in patients who have latent or active dermatitis. In pregnancy, only cryotherapy or destructive techniques with cautery or hyfrecation can be used safely. Extensive vegetating masses can cover the vulva and perianal area, particularly in diabetes, pregnancy and immunocompromised patients. Differential diagnosis Secondary syphilis may also present with extensive papulosquamous lesions. Disease course and prognosis Warts may resolve spontaneously, but may persist and be resistant especially in the immunosuppressed. Investigations the diagnosis is usually clinical, but if there are atypical features it is important to exclude vulval intraepithelial neoplasia with histological examination. Patients with genital warts should also be screened for other sexually transmitted infections. Pathology the cysts are lined by a layer of mucinous epithelium Clinical features Presentation the lesions present as single or multiple lesions in the vestibule. Fibroma Epithelial implants after surgery or at fusion sites during embryogenesis Fatty tissue of labia majora Inflamed eversion of urethral mucosa Solitary or part of generalized neurofibromatosis Fibroepithelial polyps Epidermal cyst Lipomas Neurofibroma Verruciform xanthoma [1] Granular cell myoblastoma [2,3 Urethral caruncle Leiomyoma Smooth muscle of erectile tissue, round ligament or myoepithelial cells of the Bartholin duct. Not associated with uterine lesions Syringoma [4] Adenoma of eccrine sweat glands Origin Deeper connective tissue structures. Can enlarge during pregnancy Labia majora Multiple, may be pruritic Clinical features Penduculated Pathology Fibrovascular core covered by epithelium. Cellular atypia occasionally seen Acanthosis, papillomatos is and foamy macrophages in papillary dermis Small ducts with comma like tails Cutaneous endometriosis 112. Pathophysiology Pathology A welldemarcated nodule is seen that is composed of papillary processes that extend into cystic spaces. Clinical features Epidemiology Age these are most common in women of childbearing age. Presentation Pathophysiology Pathology the cyst is lined by transitional epithelium which may exhibit squamous metaplasia. Clinical features History Simple cysts are asymptomatic and the patient may simply notice a lump. Curiously, when they are multiple, all the lesions tend to develop on one side of the vulva. In most patients, the covering epidermis remains intact, but in a proportion the elevated epithelium may become ulcerated [3]. Complications and comorbidities Malignant change within a papillary hidradenoma has been reported, producing apocrine carcinoma [5] and adenosquamous carcinoma [6]. Management Differential diagnosis Benign or malignant tumours can present in a similar way. Complications and comorbidities If the cysts become infected, then this abscess leads to painful swelling. Clinical features History the lesions may be painful and patients may report a variation in size with the menstrual cycle. Presentation Epidemiology the lesions present as small, bluish nodules and common sites are the perineum or episiotomy scars and the umbilicus. There are two forms (undifferentiated and differentiated) with different aetiologies and prognostic factors. Age these are most commonly seen in young women, but children and teenagers can be affected as well. Pathophysiology Pathology the histological features of these lesions can be difficult to interpret [2].
Chromate sensitivity from leather diabetes definition and causes buy generic forxiga on-line, and rubber allergy from elastic, may present as truncal eczema. Dermatitis from dresses, blouses and sweaters predominantly affects the neck and folds of the axilla, and spare areas of skin covered by undergarments. Outdoor workers sensitized to Compositae (Asteraceae) plants may have a diffuse dermatitis or dermatitis of an airborne pattern, which affects all the exposed areas, including the trunk if they remove their clothing to work. Detergents and fabric conditioners are commonly blamed for truncal skin eruptions but objective confirmation is usually lacking [31]. Diffuse papular eczema may be a feature of medicament sensitivity with secondary spread. There is often experimentation with a wide range of prescribed and overthecounter medicaments for pruritus, skin eruptions and haemorrhoids, and many of these contain sensitizers, most commonly fragrance, local anaesthetics and balsam of Peru (Myroxylon pereirae). Other sensitizers prescribed by the medical profession include neomycin, hydroxyquinolines, ethylenediamine, corticosteroids and topical antifungals. Moist toilet tissues and wipes may contain unnecessarily high levels of preservative, which have been associated with an increased prevalence of allergic sensitivity and in particular methylisothazolinone [32]. Nylon dyes, especially in tights, may also produce allergic contact dermatitis largely confined to this area. The ingestion of contact allergens may cause pruritus ani, particularly if they are excreted unchanged. Cashew nut oil in butter was found to induce perianal dermatitis in an individual allergic to the crosssensitizing allergenic urushiol found in poison ivy [34]. Many studies in women have not distinguished an anogenital pattern from dermatitis confined to the perianal or vulval area, but allergic contact dermatitis confined to the vulva appears to be less common [35]. Medicaments used for vaginitis rarely provoke allergic reactions on the mucosa but sometimes produce a rash on the adjacent skin, and may cause connubial dermatitis in sexual partners. Medicament allergy has frequently been associated with vulval dermatitis [36,37], and in another study investigating pruritus vulvae without associated inflammation, 49% had one or more relevant allergic reactions on patch testing, as did seven of 16 patients with lichen sclerosus. In over 50% of these patients, symptoms improved significantly or resolved when avoidance measures were taken [38]. Perfumes or antiseptics in soaps, sprays or sanitary pads are rare causes of genital dermatitis, although feminine hygiene sprays may cause both irritant and allergic reactions. Rubber accelerators in condoms can be a cause of genital eczema or pruritus vulvae. Genital dermatitis from the transfer of material carried on the hands may occur in carpenters and cabinet makers and those who work with resins. Textile dermatitis starts at the edge of the underwear, and is usually more pronounced in the popliteal spaces or gluteal folds. Allergic contact dermatitis from medicaments and dressings predominate, especially in those with varicose eczema and ulcers. The common medicament allergens are topical antibiotics and components of creams and paste bandages, such as lanolin, cetostearyl alcohol and preservatives [41]. Allergy seems to occur readily to materials that are rarely problematic in other sites. Allergy to colophony and derivatives may occur from dressing adhesives, and nylon dye allergy may be seen from hosiery. Rubber boots provoke dermatitis either at their upper edge or on the calf in areas of greatest friction. Dermatitis may result from shoe materials including leather, rubber, glues and nickel, stockings, topical medicaments, antiseptics and antiperspirants. Generalized erythroderma may be the result of a chronic contact dermatitis maintained by continued exposure to a wide range of allergens, including components of topical medicaments. Exposed sites Contact dermatitis from dust, sprays, pollens or volatile chemicals is typically confined to the exposed surfaces of the hands, arms, face and neck. There is great diversity in the nature of airborne reactions, which may be irritant, allergic, phototoxic, photoallergic or contact urticarial. Discount forxiga 10 mg with visa. HEAL NEUROPATHY WITH NUTRITIONAL SUPPLEMENTATION - Dr Alan Mandell DC.
|