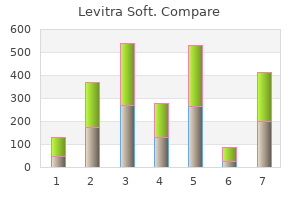
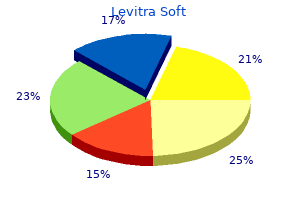
Levitra Soft"Levitra soft 20 mg on-line, erectile dysfunction doctors in maine". By: W. Aschnu, M.B.A., M.B.B.S., M.H.S. Program Director, University of New England College of Osteopathic Medicine Cough is generally produced by a reflex response arising from irritant receptors located in ciliated epithelia in the lower respiratory tract erectile dysfunction treatment auckland levitra soft 20 mg without a prescription, but it can be suppressed or initiated at higher cortical centers. One of the most common causes of cough in pediatric patients is the self-limited cough of an acute viral lower respiratory illness or bronchitis that lasts 1 to 2 weeks. A diagnostic approach to chronic cough is best served by considering the age of the child (Box 17. The chest radiograph is nondiagnostic and can be normal or show perihilar infiltrates. A high white blood cell count with a predominance of lymphocytes supports the diagnosis, but unfortunately once the patient has passed through the usually innocent-appearing coryzal stage into the paroxysmal stage, diagnostic tests have a lower yield. Ureaplasma urealyticum and Pneumocystis jiroveci (formerly known as Pneumocystis carinii) have been recognized as causes of pneumonia and persistent cough in this age group. Chronic aspiration is a cause of respiratory symptoms that should be considered, particularly in medically complex infants. Age and Cause Infancy (Younger Than 1 Year Old) Cough starting at birth or shortly afterward may be a sign of serious respiratory disease and must be evaluated assiduously. Cough beginning at this time raises the possibility of congenital infections, such as cytomegalovirus or rubella, which are often associated with other findings, such as hepatosplenomegaly, thrombocytopenia, or central nervous system disease. A, Anteroposterior chest radiograph shows feeding tube passing no farther than proximal esophagus; there is an aspiration pneumonitis present. B, Lateral view showing the feeding tube in the proximal esophageal pouch with air in the airway, distal esophagus, and intestine. Aspiration may be due to neurologic, anatomic, or functional disorders, often with a combination of factors present. Infants with neurologic disorders may have incoordination of swallowing and sucking reflexes that lead to aspiration of milk or gastric contents, as well as saliva into the lung. These anomalies are associated with feeding-related coughing, choking, and occasionally cyanosis or persistent hypoxemia. Congenital thoracic malformations may also present as persistent or recurrent cough, wheeze, or pneumonias. Diagnoses within this category include bronchial atresias or hypoplasia, bronchogenic cysts, congenital pulmonary adenomatoid malformations, as well as sequestrations (see Chapter 18). Pulmonary sequestration (in which a portion of the lung is perfused by systemic, not pulmonary, arteries). Right-sided or double aortic arch, innominate artery compression, and pulmonary artery slings are a few of the many potential lesions. Aberrant major blood vessels generally cause inspiratory stridor and expiratory wheezing from tracheal compression, but a brassy cough may also be observed, as may dysphagia from the associated esophageal compression. B, Aortic angiogram demonstrates anomalous origin of pulmonary blood supply from abdominal aorta to the left lower lobe in a 7-year-old girl with extralobar sequestration. Asthma (formerly called reactive airway disease) or bronchial hyperresponsiveness is a common and probably underdiagnosed cause of cough in infancy. Cough or persistent wheezing can be found in these infants, who may have a history of a previous viral lower respiratory illness with or without a family history of wheezing and/or asthma. These disorders usually involve the pulmonary interstitium but can involve other aspects of lung parenchyma. A further category of lung disease where infants may present with variable symptom severity is congenital pulmonary lymphangiectasia. This disease is characterized by dilated pulmonary lymphatic vessels with associated disordered drainage. Lymph builds up within the lungs, leading to respiratory symptoms, such as recurrent cough, wheeze, hypoxemia, or tachypnea. Lymphatic involvement may be isolated to the lungs or involve multiple organ systems. Postnatally, chylothoraces are present with associated pulmonary hypoplasia leading to respiratory failure. Although the exact incidence of pulmonary lymphangiectasia has not been determined, it is believed that up to 1% of infants who die in the neonatal period may be afflicted. Although the majority of cases are believed to present in infancy, reports of older children or adults with a milder spectrum of symptoms have also been reported. Pulmonary lymphangiectasia may be seen in two categories: in the setting of a primary developmental defect, or secondary to an impedance of normal lymphatic flow. In other cases erectile dysfunction treatment bangalore levitra soft 20mg low price, there is widespread breakage at the scalp, creating a "salt-and-pepper" appearance, with the short residual hairs appearing as black dots on the surface of the scalp. In yet other children, sensitization to the infecting organism results in more erythema, edema, and pustule formation. As the latter rupture, the area weeps and golden crusts form, simulating impetigo. Some cases are characterized by patches of heaped-up scale in association with small pustules. Less commonly, intense inflammation causes formation of raised, tender, boggy plaques or masses studded with pustules that simulate abscesses, termed kerions. Unless treated promptly and aggressively with oral antifungal agents and, in cases characterized by severe inflammation, systemic steroids, the latter may produce scarring and permanent hair loss. Incision and drainage of kerion is not indicated, because loculations are small and septae thick. Importantly, when pustules or weeping and crusting lesions involve the scalp or hair line, the infection is far more likely to be of fungal than bacterial origin. Patients with tinea capitis often have associated occipital, postauricular, and posterior cervical adenopathy. In the past, when Microsporum audouinii was the most common causative organism and was easily identified by its fluorescence, the Wood lamp was a useful adjunct in diagnosis. A negative Wood lamp exam, however, will not rule out the most common cause of tinea capitis. Because topical antifungal agents do not penetrate deeply enough to be effective in the treatment of tinea capitis, oral antifungal agents are necessary and must be administered for at least 6 weeks to eradicate the infection. Studies show that itraconazole and fluconazole are also effective and require shorter (6-week) courses of therapy. However, reports of severe adverse side effects of ketoconazole have sharply curtailed its use, and studies of this agent have also raised concerns about its efficacy. Other measures useful in reducing passage of organisms to others include avoidance of communal use of brushes, combs, or hair grease jars, hats, coats, scarves, towels, or linens; and careful washing or cleaning of combs and brushes and of potentially contaminated linen, clothing, and upholstery. Scarring Alopecia Scarring alopecia is considerably less common than nonscarring alopecia in children and may be caused by a number of disorders, both congenital and acquired. On examination, no intact hair follicles are seen in the areas of alopecia due to permanent scar formation. Morphea (localized scleroderma) and lupus may involve the scalp with indurated, hairless plaques. Aplasia Cutis Congenita Aplasia cutis congenita is a congenital condition characterized by absence of or failure of formation of a localized area of epidermis, dermis, fat, bone or some combination of these layers. Rarely they may be associated with limb defects and other congenital and genetic anomalies. In the majority of cases, only the dermis and epidermis are absent; however, some lesions extend to involve subcutaneous tissue, and, in rare cases, a calvarial defect may underlie a scalp lesion, which is why deep palpation of more extensive lesions is discouraged until imaging has been performed. At birth, the lesion may consist of a sharply circumscribed open and weeping erosion or ulceration, or it may be covered by a thin, often hemorrhagic membrane or crust. Evaluation should include radiologic studies to assess the depth of the lesion and a search for associated anomalies. A, In this child, mild erythema and scaling of the scalp are associated with spotty alopecia. B, Infiltration of hair shafts by an endothrix fungus has resulted in widespread breakage at the scalp, producing a "salt-and-pepper" appearance. C, Superficial papules and pustules have ruptured, producing weeping and crusting lesions simulating impetigo. This child, seen relatively late in the course, had nearly total alopecia over the involved area. Conservative treatment designed to protect the area from infection and injury includes application of topical antibiotics. Generic 20 mg levitra soft with amex. Survival of the Firmest: Erectile Dysfunction and Death.
The retinopathy of rubella syndrome is a diffuse "salt and pepper" retinopathy that develops early in childhood and does not affect vision impotence legal definition discount levitra soft 20mg without prescription. The pigmentary changes may be similar in appearance to those of syphilis, retinitis pigmentosa, and Leber congenital amaurosis. Retinitis, with hemorrhages and perivascular yellowish-white exudates secondary to cytomegalic inclusion disease. Other ophthalmic manifestations include microphthalmia, uveitis, cataracts, optic disc atrophy, strabismus, and nystagmus. Retinal inflammation, edema, and hemorrhage may be extensive and rapidly progressive in these patients. Herpes Simplex Virus Herpes simplex virus infection may involve the anterior segment of the eye, with conjunctivitis, keratitis, and iritis or, especially when disseminated in the perinatal period, a retinochoroiditis may develop. Retinal involvement with disseminated herpes simplex virus is severe, with extensive inflammatory reaction producing yellowish-white exudates and retinal necrosis. Herpetic retinitis may occur in normal individuals but is more common in the immunosuppressed. Syphilis Congenital syphilis may cause bilateral chorioretinitis, resulting in a salt-and-pepper fundus appearance. Differentiation of the retinopathy of congenital syphilis from retinitis pigmentosa may be difficult. Syphilis may also cause interstitial keratitis, anterior uveitis, glaucoma, and optic nerve atrophy. Toxocariasis Toxocara canis larvae infect children most commonly from 2 to 9 years old. Chronic unilateral uveitis with opacification of the vitreous overlying the granuloma may occur. Inflammation in ocular toxocariasis occurs only after the infecting organism dies. Externally, the eye does not appear to be inflamed and diagnosis is usually made when investigating absence of the red reflex, strabismus, or decreased vision. With extensive inflammation, fibrotic preretinal membranes may develop and produce retinal detachment. There are small flame-shaped hemorrhages within the nerve fiber layer that follow the pattern of the retinal vessels. More extensive areas of hemorrhage have broken through to the preretinal space and are seen as areas of blood that obscure the retina. A Roth spot, that is, a hemorrhage with a white center, is visible just above the optic disc. The white reflection from the camera flash is visible because of dispersed red blood cells within the vitreous. Septic emboli cause intraretinal hemorrhages, which are flame shaped or dot-blot like in nature. If the hemorrhage has a white center from the accumulation of leukocytes, the term Roth spot is used. Occlusion of the central retinal artery causes a sudden profound loss in vision, loss of the pupillary reaction to light, absence of venous pulsations, and the development of a cherry-red spot in the fovea. Edema and opacification of the ganglion cell layer surrounding the fovea make the fovea stand out as red to produce this sign. Prognosis with treatment even when provided virtually immediately with the episode is poor. Bacterial Endocarditis Cotton-wool spots are small white, irregular retinal lesions caused by infarction of the retinal nerve fiber layer. They may be seen in any condition that produces retinal ischemia, such as hypertension and diabetes (rarely in the pediatric age population), or in patients with acquired immunodeficiency syndrome. Cotton-wool spots Leukemia Patients with acute lymphoblastic, myelogenous, or monocytic leukemia may develop flame-shaped intraretinal hemorrhages. Leukemic infiltration may also occur in the retina as a perivascular infiltrate in the choroid or in the optic disc, producing disc swelling and a papilledema-like appearance. Leukemic involvement of the orbit may be difficult to distinguish from bacterial orbital cellulitis. Diabetes the most common ocular finding in young diabetic patients is transient lenticular myopia. This increases the lens osmolarity and causes the lens to swell, producing myopia.
To avoid confusion erectile dysfunction medications otc 20mg levitra soft for sale, the canal should be inspected as the speculum is inserted to ensure that the transition between canal wall and tympanic membrane is visualized. The pneumatic otoscope is the most valuable diagnostic tool when signs or symptoms of otitis media are present. Pediatricians, family practitioners, and otolaryngologists who treat children should be skilled in its use. Replace bulbs routinely every 4 to 6 months, and provide for routine battery charging. When otoscopic findings are unclear or when it is difficult to obtain a good air seal for pneumatic otoscopy, tympanometry can be highly useful in evaluating patients older than 8 months old. The procedure is of lesser value in young infants because the abundance of loose connective tissue lining the ear canal and the laxity of the cartilage at the entrance increase canal wall compliance and invalidate the results. Because otitis media can be a reflection of both immunologic and anatomic abnormalities, the practitioner should be suspicious of possible underlying immune or temporal bone defects when seeing he importance of pediatricians and family physicians having an understanding of and experience with otolaryngologic problems and being skilled in techniques of examination of the head and neck region cannot be overemphasized. When nasal and oral symptoms are included, ear, nose, and throat pathology accounts for more than 50% of all visits. With patience and proper equipment, pediatricians can complete a thorough examination on almost all children. If a disorder fails to respond to therapy or becomes chronic or recurrent, or if an unusual problem is encountered, then consultation with a pediatric otolaryngologist should be sought. Successful examination of the ears, nose, and oropharynx of a young child can present some challenges, especially with older infants and toddlers. This can be a particular problem in children who have had previous bad experiences. Patience, warmth, humor, and careful explanation on the part of the examiner help reduce fear and enhance cooperation. Gradual introduction of the equipment can also be helpful, especially if done in a playful way. Parents can also help demonstrate maneuvers for opening the mouth, panting to depress the tongue, and holding the head back. Although this may take a little additional time at the outset, it often saves considerable time in the long run and makes future follow-up examinations far easier. Less specific symptoms such as pulling or tugging at the ears, fussiness, and fever are also frequently encountered, particularly in children younger than 2 years old. History should center on the nature and duration of symptoms, character of the clinical course, and possible antecedent treatment. Because many infections of the ear are recurrent and/or chronic, the parent should be asked about previous medical or surgical therapy. A brief review of the anatomy of the ear is helpful in developing a logical approach to any clinical abnormalities that may be encountered. The external ear includes the pinna, or auricle, and the external auditory canal, up to and including the tympanic membrane. The middle ear is made up of the middle ear space, the inner surface of the eardrum, the ossicles, and the mastoid. The inner ear comprises the cochlea (hearing), the labyrinth and semicircular canals (balance), and the main nerve trunks of the seventh and eighth cranial nerves. C and D, Making a game of blowing out the otoscope light and allowing the patient to check the examiner first convey that otoscopy does not have to hurt. A, A normal external ear (auricle or pinna) is shown, with its various landmarks labeled. B, this coronal section shows the various structures of the hearing and vestibular apparatus. The eustachian tube connects the middle ear and the nasopharynx and serves to drain and ventilate the middle ear. Additional implements include cotton wicks (3) and a suction tip (4) for removal of discharge or moist wax, alligator forceps (5) for removing foreign bodies, and an ear syringe (6) and motorized irrigation apparatus (7) for removing firm objects or impacted cerumen. Lavage is contraindicated when there is a possible perforation of the tympanic membrane. If the motorized apparatus is used for irrigation, it must be kept on the lowest power setting to avoid traumatizing the eardrum. C, Allowing the child to look through the examining microscope may help him or her cooperate with the examination.
|