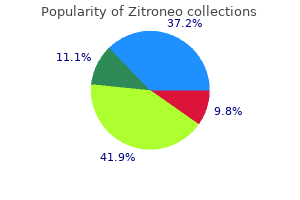
Zitroneo"Purchase cheap zitroneo line, infection in the blood". By: J. Hamid, M.B. B.CH. B.A.O., Ph.D. Clinical Director, Loyola University Chicago Stritch School of Medicine Closed nailing was done in this patient antibiotics in copd exacerbation discount zitroneo 500 mg without prescription, however, and tumor progression (despite radiation) resulted in unavoidable hardware G breakage. Similar outcome with uncemented fixation of metastatic renal cell carcinoma of the subtrochanteric region. Surgery should include meticulous tumor removal and filling of the entire tumor cavity with bone cement. Function after resection of humeral metastases: analysis of 59 consecutive patients. Impending and actual pathological fractures in patients with bone metastases of the long bones: a retrospective study of 233 surgically treated fractures. Impending pathologic fractures from metastatic malignancy: evaluation and management. Comparison between solitary and multiple skeletal metastatic lesions of breast cancer patients. Metastatic disease in long bones: a proposed scoring system for diagnosing impending pathologic fractures. Surgical treatment of skeletal metastatic lesions of the proximal femur: endoprosthesis or reconstruction nail A study of the surgical treatment of 166 pathological humeral and femoral fractures. Chapter 6 Cryosurgical Ablation of Bone Tumors Jacob Bickels, Isaac Meller, Yehuda Kollender, and Martin M. It is an intralesional procedure, which permits the avoidance of major resection and associated loss of function. It weakens the bone surrounding the tumor cavity and, when not used judiciously, may cause additional soft tissue injuries. Awareness of these potential complications has led to refinement of surgical practices to include soft tissue protection, stable reconstruction, the use of perioperative antibiotics, and enhancement of rehabilitation protocols for gradual weight bearing. Those guidelines have resulted in a gratifyingly low rate of complications and rendered this treatment a safe and reliable modality. It may be expected that cryoablation will no longer be the exclusive practice of a relatively small group of surgeons and that it will eventually enjoy greater popularity in the not too distant future. Historical Aspects and Physiologic Background Although cryoablation had been used in the 1850s for the management of locally advanced carcinoma of the cervix, its applicability to the management of bone tumors was not assessed until more than a century later, in the classic 1966 animal study by Gage et al,13 in which the femora of living mongrel dogs were frozen by perfusing liquid nitrogen through encircling latex coils. Using histopathologic studies and plain radiographs, the authors documented the occurrence of tissue necrosis and bone resorption that was associated with mechanical weakening and spontaneous fractures. They further suggested the use of intralesional cryoablation in lieu of tumor resection or amputation. Four mechanisms are involved in the immediate cytotoxicity produced by cryoablation: (1) formation of ice crystals and membrane disruption; (2) thermal shock; (3) dehydration and toxic effects of electrolyte changes; and (4) denaturation of cellular proteins. The formation of intracellular ice crystals is considered as being the main mechanism of immediate cellular necrosis. The two mechanisms most likely responsible for the delayed, progressive necrosis that is observed following cryoablation and for the problems associated with subsequent repair of frozen tissue are (1) the damage to the microvascular circulation and (2) vascular stasis. The withdrawal of water from the system into these crystals creates a hyperosmotic extracellular environment, which, in turn, draws water from the cells. As the process continues, these crystals grow, the cells shrink and dehydrate, electrolyte concentration is increased, and membranes and cell constituents are damaged. Conversely, a slow thaw will cause intracellular recrystallization of the already formed crystals and membrane disruption, whereas a rapid thaw will not. Histologically, the most dramatic effect of cryoablation is on the appearance of the bone marrow: a rim of 1 to 2 cm of extensive necrosis with minimal inflammatory response appears following direct pour of liquid nitrogen. General anesthesia is reserved for extremely long cases and is combined with brachial plexus analgesia antimicrobial proteins purchase zitroneo online now. Carpel tunnel release surgery is one of the most common hand procedures and may be done with an intravenous regional block (Bier block). Local infiltration by the surgeon combined with intravenous sedation is a more common and efficient anesthetic approach. The nerves in the axilla have a predictable anatomic relationship to the axillary artery. The block may be done with paresthesia, nerve stimulation, or transarterial approaches. Continuous peripheral nerve catheters may be placed if the procedure is prolonged, a sympathectomy is needed, or significant pain is expected. Brachial plexus anesthesia with an intercostobrachial nerve block will prevent tourniquet pain, unlike general anesthesia. Supplementing Nerve Blocks It is preferable to place blocks outside the operating room so that block efficacy can be evaluated. Often a "failed" block is simply the result of inadequate time for local anesthetic distribution to nerve targets. Insufficient blocks can be supplemented, and again ultrasound offers a safe option for this. Propofol infusions will allow control of anxiety and can turn an incomplete block into an intraoperative success. Sterile ultrasound probe and needle insertion for sonographically guided axillary block. Continuous Nerve Blocks Postoperative pain control after a single injection of local anesthesia is limited to 16 hours, and this limits its usefulness for postoperative pain management. Because of the anatomic relationships of the upper extremity, a single catheter may provide continuous analgesia in the distribution of surgical pain. The surgical pain is not amplified at the tissue level or centrally in the spinal cord, so the pain is less intense and of shorter duration. Patients must be counseled about the danger of injury in the absence of normal pain responses. When continuous peripheral nerve catheters are part of a multimodal pain therapy consisting of nonsteroidal antiinflammatory medications, acetaminophen, cryotherapy, and weak opioids, greater analgesia and patient satisfaction may be achieved. The efficacy of continuous interscalene blocks was demonstrated in patients treated with ropivacaine 0. The blocks were associated with less pain, resulting in fewer sleep disturbances, less opioid consumption, and fewer side effects. Local anesthetic toxicity is most likely during the initial injection (bolus with 30 to 40 cc of bupivacaine or ropivacaine 0. Local Anesthetics and Additives Local anesthetics produce anesthesia by inhibiting excitation of nerve endings and blocking conduction in peripheral nerves due to the binding and inactivation of both sodium and potassium channels. This prevents the sodium influx through these channels that is necessary for the depolarization of nerve cell membranes and propagation of impulses along the course of the nerve. There are two classes of local anesthetics, named for their linkage between the carbon chain and aromatic chain. The amino esters are metabolized in the plasma via pseudocholinesterases, and amino amides are metabolized in the liver. Amino esters are eliminated rapidly compared with amides, decreasing the possibility of toxicity. Amino esters are much more likely than amino amides to cause true allergic reactions due to metabolites like para-aminobenzoic acid. Toxicity from local anesthesia occurs when a peak plasma level is reached, typically from inadvertent intravascular administration of anesthetic. Toxicity from rapid absorption is also possible, especially in vascular areas (intercostal, epidural, or interscalene), and epinephrine is added to the local anesthetic to signal intravascular injection and decrease the vascular absorption of the local anesthetic. Because of their potent binding to the heart, these arrests can be difficult to treat. Cardiotoxicity from bupivacaine has been successfully treated with 2 mL/kg of 20% lipid emulsion in a case report. Generic zitroneo 250mg without a prescription. HOW TO Install Slow Close Toilet Seat ~ INSTALLATION Walk Through Slow Close Quick Release.
Approach to the metacarpophalangeal joints Approach to the carpal tunnel If necessary bacteria zip line girl buy generic zitroneo 250mg line, release the ulnar sagittal band at the joint. Volar approach to the radius Dorsal approach to the radius Protect branches of the palmar cutaneous branch of the median and ulnar nerves in the subcutaneous tissue by centering the incision in the interthenar eminence. Remain vigilant for a transligamentous recurrent motor branch of the median nerve. Dissection should not drift ulnar to the flexor carpi radialis tendon to protect the median nerve and its cutaneous branches. The posterior interosseous nerve ends at the level of the wrist dorsally in line with the fourth metacarpal and is easily approached for denervation for postoperative pain relief. The superficial branch of the radial nerve: an anatomic study with surgical implications. Avoidance of transection of the palmar cutaneous branch of the median nerve in carpal tunnel release. Postoperative pain management represents a particular challenge with ambulatory surgery, as 40% of patients experience severe pain despite treatment. However, patients and surgeons alike become frustrated when these blocks dissipate in the middle of the night, resulting in the return of severe pain. Despite the selection of long-acting local anesthetics (14 to 24 hours of analgesia), about 20% of patients after orthopaedic surgery have significant pain requiring opioids after 7 days. The frustration with the limited analgesia provided by a single dose of local anesthetic causes some physicians to avoid nerve blocks altogether. This approach is associated with increased side effects such as urinary retention, pruritus, ileus, nausea, and vomiting. If continuous regional analgesia is selected, it may be used for anesthesia and postoperative analgesia. The continuous peripheral nerve catheter offers prolonged analgesia and minimal side effects and eliminates the problem of block resolution and the return of severe pain. The nerve block is maintained with a continuous infusion of local anesthetic agents. Pumps have been developed allowing outpatient infusions, and these elastometric pumps are ideal because they are compact, simple to operate, and designed to provide safe infusion rates of local anesthetic in the uncontrolled home environment. This C1 and C2 instability may produce subluxation, resulting in cord compression and paralysis. Anatomic changes involving the cervical spine, temporomandibular joint, or arytenoids may necessitate awake airway management with a fiberoptic bronchoscope (Table 1). Preoperative flexion and extension films are indicated with advanced rheumatoid arthritis, and cervical fusion of C1 to the occiput may be required before the procedure. Regional anesthesia may avoid the airway challenges of general anesthesia, but it may be difficult in these patients if the loss of range of motion in the joints prevents proper needle placement. Rheumatoid arthritis is associated with cardiovascular disease, and atherosclerosis occurs at an accelerated rate in rheumatoid arthritis, resulting in a greater risk of myocardial infarction and cerebrovascular accident. Trauma Surgical emergencies may require general anesthesia before completing radiologic evaluations. Factors that influence this decision include surgery on more than one extremity, unknown duration of procedure, the need to assess postoperative neurologic function, and surgeon or patient preference. Regional anesthesia may be performed in a child during general anesthesia, but the loss of patient feedback regarding pain and paresthesia increases the risk of neural injury. Regional anesthesia decreases anesthetic and opioid requirements, resulting in shorter wakeup times with general anesthesia. Caudal and spinal blocks have been the most commonly used regional techniques due to the anesthesiologist familiarity and their relative safety when performed in the anesthetized patient. Nerve blocks may provide preemptive analgesia by blocking painful stimuli and lead to lower stress hormone levels and less overall pain. Pediatric regional techniques require smaller needles, which have only recently become available, but continuous blocks are done with adult equipment, a less-than-optimal situation. Pediatric patients require cautious local anesthetic selection and administration to avoid toxicity.
Scapholunate ligament repair and capsulodesis for the treatment of static scapholunate dissociation virus software zitroneo 100mg low price. A survey of the surgical management of acute and chronic scapholunate instability. It may appear either as an isolated injury, or associated with distal radius fractures or displaced scaphoid fractures. The dorsal scapholunate ligament is formed by dense, slightly oblique connective fibers that link the dorsal aspects of the scaphoid and lunate bones. If the scapholunate ligaments are completely torn, the scaphoid no longer appears constrained by the rest of the proximal row, and tends to collapse into an abnormally flexed and pronated posture ("rotatory subluxation of the scaphoid"). Both the lunate and the distal row have been drawn away from the scaphoid to better expose the ligaments. If left untreated, a partial scapholunate tear may progress toward a more complete disruption of all three elements of the scapholunate joint, in which case a symptomatic dysfunction usually appears. Under axial load (blue arrows) the scaphoid tends to rotate into flexion (red arrows) while the triquetrum tends to extend. If both the scapholunate and lunotriquetral ligaments are intact, the two opposite moments counteract each other and a stable equilibrium is reached, allowing force to be transmitted across the proximal row. If the scapholunate ligaments fail and the secondary stabilizers do not succeed in maintaining the scaphoid aligned, a diastasis appears between the scaphoid and lunate (red arrow). This gap is formed as the consequence of the capitate edging into that space (blue arrow), forcing the proximal scaphoid to subluxate over the dorsal edge of the distal radius. In such circumstances, the lunate follows the triquetrum into further extension (dorsal intercalated segment instability) and ulnar translation. The abnormal joint contact between radius and scaphoid may cause cartilage deterioration of the proximal pole of the scaphoid and the reactive formation of an osteophyte at the tip of the radial styloid. One is the patient who presents following violent trauma, such as a fall from a height or a motorcycle accident, who is likely to have a major carpal derangement. Another is the patient who may not recall specific trauma and yet presents with symptoms. In the second case, identification of the true nature of dysfunction may require a high index of suspicion, careful examination, and appropriate diagnostic tools. Not uncommonly, arthroscopy is the only way to fully assess the extent of ligament derangement (see Chap. In acute cases, range of motion may be limited by pain, whereas it may be normal in chronic cases. Scapholunate point tenderness: If sharp pain is elicited by pressing this area, the probability of localized synovitis is high. The resisted finger extension test9 has low specificity but excellent sensitivity. In the presence of scapholunate injury, sharp pain is elicited at the scapholunate area, representing dorsal subluxation of the scaphoid. Scaphoid shift test9: If the scapholunate ligaments are completely torn, the proximal pole may sublux dorsally out of the radius, inducing pain on the dorsoradial aspect of the wrist. This test has low specificity: occult ganglia, hyperlaxity, or radioscaphoid degenerative arthritis may produce similar symptoms. Three-ligament tenodesis for the treatment of scapholunate dissociation: Indications and surgical technique. A foreshortened appearance of the scaphoid with the scaphoid tuberosity projected in the form of a ring over the distal two thirds of the scaphoid (ring sign) indicates rotatory subluxation of the scaphoid. Lateral radiographic view Increased scapholunate angle compared with the contralateral side. For this to be significant, the wrist needs to be in strict neutral alignment and neutral prono-supination. It is also useful in describing the degree of injury to the interosseous ligaments. Complete disruption of scapholunate ligaments, the dorsal one being still reparable, with good healing potential. Its contraction generates a dorsally directed vector to the unstable scaphoid that prevents its collapse into flexion.
|