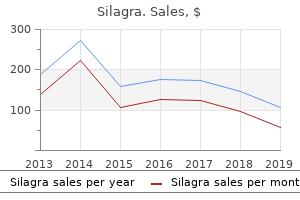
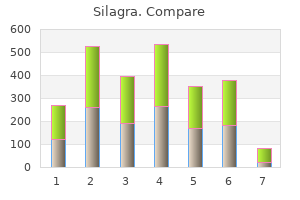
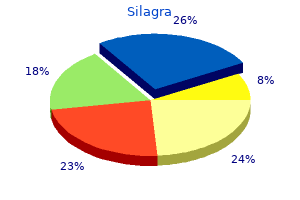
Silagra"Silagra 100mg without prescription, erectile dysfunction drugs australia". By: M. Tragak, M.S., Ph.D. Clinical Director, Florida State University College of Medicine Clinical features Patients may present in infancy with jaundice erectile dysfunction doctors in lafayette la purchase silagra 50mg line, hepatomegaly, splenomegaly, and acholic stools. Patients with truncated proteins secondary to homozygous nonsense mutations present early, while homozygous or heterozygous missense mutations present later. Liver disease tends to evolve slowly to biliary cirrhosis with or without overt cholestatic jaundice. Esophageal varices were found in 19 patients at a mean age of 9 years (range, 5Ͳ0. Asymptomatic disease leading to cirrhosis, portal hypertension, and variceal bleeding in adolescent and young adults has also been reported. Affected patients suffer from symptomatic cholesterol cholelithiasis, usually before age 40 years, along with intrahepatic sludge and microlithiasis [46]. These patients experience symptom recurrence, even after cholecystectomy, because of intrahepatic cholesterol deposits and bile duct inflammation. A predisposition to develop gallstones in these patients is not surprising as phospholipids are the main carrier and solvent of cholesterol in hepatic bile [46]. They develop generalized pruritus, rarely accompanied by jaundice, which is exacerbated late in gestation. These women may have subclinical or symptomatic steatorrhea, with weight loss and fat-soluble vitamin deficiencies. Serum alanine aminotransferase and bile acid concentrations are increased, while bilirubin is typically normal. Most concerning, however, is the significant risk intrahepatic cholestasis of pregnancy carries for the fetus, with high rates of prematurity and risk of fetal distress or stillbirth, often after 35 weeks of gestation [44]. Cholestasis recurs in 60ͷ0% of subsequent pregnancies and may also occur during administration of oral contraceptives [48]. Fluctuation in both estrogen and progesterone may contribute to the symptomatic presentation, as evidenced by symptom development late in gestation, when hormone levels are high, resolving after delivery when hormone levels return to baseline, and being more frequent in twin pregnancies, in which higher hormone levels are present [44]. Prenatal mutation analysis in kinships known to be affected by intrahepatic cholestasis of pregnancy is available. Other commonly used liver tests are variably elevated, including serum aminotransferases (5 times normal), conjugated bilirubin (2 times normal), and alkaline phosphatase (2 times normal). The total serum bile acid concentration is elevated to as high as 25 times the normal value, but biliary bile acid concentrations are normal [42,44]. Portal zone at the left shows bile ductular proliferation and mild mixed inflammatory infiltrate. Inflammatory cells include lymphocytes, plasma cells, and occasional polymorphonuclear leukocytes. Ratios of biliary bile acid to phospholipid and cholesterol to phospholipid were approximately five-fold higher than in control samples. Lipoprotein X is the predominant lipoprotein in the plasma of cholestatic patients. Lipoprotein X is probably composed of biliary vesicles that are formed at the subapical compartment of the hepatocyte, transcytosed to sinusoidal membrane, and released into plasma. Cholestasis with giant cell transformation and isolated eosinophilic necrotic hepatocytes may also be present. Eleven missense mutations and six mutations predicted to yield a truncated protein were identified. The high biliary cholesterol saturation index promotes crystallization of cholesterol and the lithogenicity of bile. The Mdr2/ mice developed a cholangiopathy characterized histologically by bile ductular proliferation, portal inflammation, and progressive fibrosis. These mice had low to absent concentrations of biliary phosphatidylcholine but maintained normal bile salt secretion. The bile salt export pump moves bile salts from the hepatocyte into the canalicular lumen. Mixed bile salt/phosphatidylcholine/cholesterol micelles move down the biliary tract into the gallbladder and duodenum. These mixed micelles are thought to protect the canalicular and cholangiocyte membranes from bile acid-induced cell injury. There was disruption of tight junctions and basement membranes, with bile acid leakage into portal tracts of Mdr2/ but not wild-type mice. These mediators resulted in activation of periductal myofibroblasts, producing periductal fibrosis, the separation of the peribiliary plexus from cholangiocytes, and eventually atrophy and death of the cholangiocytes.
Manifestations of cholestatic liver disease in the neonate Jaundice is the most overt physical sign of liver disease and occurs more commonly in the neonatal period than at any other time of life [20] cialis erectile dysfunction wiki buy silagra 50 mg with mastercard. Unconjugated hyperbilirubinemia in the older patient is usually harmless, but in the neonate with an immature bloodrain barrier, it may be associated with deposition of free bilirubin in neuronal tissue and subsequent brain damage. In contrast, conjugated bilirubin is not toxic, but an elevated level is the most common presenting feature of liver disease in the neonate. Unconjugated jaundice is first appreciated in the head and progresses caudally to the palms and soles as the serum bilirubin increases. Jaundice becomes clinically apparent in the older child when the serum bilirubin concentration reaches 2ͳ mg/dL, but the neonate may not appear icteric until the bilirubin level is >5 mg/dL. A serum conjugated (direct) bilirubin concentration of >1 mg/dL with a total bilirubin of <5 mg/dL, or over 20% of the total bilirubin concentration if the total is >5 mg/dL, is abnormal and requires evaluation [21]. Many clinical laboratories now employ the Ektachem method, which specifically measures direct bilirubin. The majority of infants with cholestatic liver disease present during the first month of life [13]. Differentiation of cholestatic jaundice from the common physiologic hyperbilirubinemia of the neonate or the prolonged jaundice occasionally associated with breast-feeding is essential. The initial goal of the physician must be to exclude rapidly life-threatening but potentially treatable disorders such as Gram-negative infection, endocrinopathies (such as panhypopituitarism), galactosemia, and inborn errors of bile acid metabolism. Prompt identification of cholestatic infants is also required to minimize the risk of hemorrhage from vitamin K deficiency. The possibility of liver or biliary tract disease must be considered in any neonate jaundiced beyond 2 weeks of age. These infants should be evaluated for cholestasis by measurement of total and conjugated serum bilirubin. However, with reliable followup, this testing may be deferred until 3 weeks of age in jaundiced breast-fed infants if stool color, urine color, and physical examination are normal. In one study, the incidence of jaundice in breast-fed babies at 4 weeks was 9%, but none had liver disease [22]. In a community-based study in which 27 654 neonates were tested for a serum conjugated bilirubin concentration >18 mol/L using the Ektachem method, a positive result requiring further testing was found in 107 babies. Persistently elevated values on repeat testing was seen in 12 babies, 11 of whom had confirmed liver disease including neonatal hepatitis (six), biliary atresia (two), hypopituitarism (one), 1-antitrypsin deficiency (one), and Alagille syndrome (one). General application of this approach will likely require methods to measure conjugated bilirubin on dried blood spots. In Taiwan, a national screening program has been implemented through which an infant stool color card is placed into the child health booklet given to every neonate. This program has increased the national rate of the Kasai operation performed before 60 days of age from 49% to 66%, and it has increased the 3-month jaundice-free rate after the Kasai operation from 35% to 61% (p < 0. In addition, the 5-year jaundice-free survival rate with native liver increased from 27% to 64% (p < 0. The vast majority of infants with biliary atresia appear entirely well during the first 4Ͷ weeks of life apart from mild jaundice. However, the apparent well-nourished appearance of infants with biliary atresia may be a factor in a delay of diagnosis. Thorough anthropometric studies show that infants with biliary atresia have significantly decreased fat stores and lean body mass [25]. The added weight of an enlarged liver and spleen and the occasional finding of subclinical ascites may account for a relatively normal weight for age and weight for length on standardized growth curves [26]. Stools of a patient with biliary atresia are acholic, but early in the course of incomplete or evolving obstruction, stools may appear normally pigmented or only intermittently pigmented. Similarly, fluctuating levels of serum bilirubin do not eclude biliary atresia [27]. Liver disease also must be suspected in a jaundiced infant whose urine is dark yellow as opposed to colorless. Lack of follow-up of neonatal jaundice, inadequate investigation of hemorrhagic disease, misdiagnosis of breast milk jaundice, and being misled by pigmented stools or a decrease in serum bilirubin were cited as reasons for late referral. Increased age at Kasai operation has been shown to be associated with worse survival, independent of other prognostic factors. In a recent study of 695 patients with biliary atresia who underwent the Kasai procedure in France, survival with native liver was best in children operated on in the first 30 days of life [28]. A stepwise discriminate analysis by Alagille [29] of many clinical and biochemical findings identified several variables that are useful in evaluating the cholestatic infant. A report of risperidone hepatotoxicity in two children may actually have been concurrence of non-alcoholic steatohepatitis and drug toxicity [206] causes of erectile dysfunction in 20s purchase cheap silagra online. However, it has become evident that severe liver injury may occur in some children [208]. Children taking risperidone should have serum aminotransferases and bilirubin monitored regularly; tracking body mass index and waist circumference may also be worthwhile. Sulfanilamide, trimethoprimγulfamethoxazole, and pyrimethamine-sulfadoxine have all been reported as causing significant hepatotoxicity [209]. Sulfasalazine has been associated with severe liver disease in adolescents and young adults, including acute liver failure, sometimes fatal [210]. The spectrum of sulfa-associated liver toxicity also includes asymptomatic elevation of serum aminotransferases [211] and granulomatous hepatitis. In general, sulfa hepatotoxicity is associated with a systemic drug hypersensitivity reaction. Fever, significant rash, periorbital edema, atypical lymphocytosis, lymphadenopathy, and renal dysfunction with proteinuria all may occur; myocarditis may be prominent. Dapsone resulting in acute liver failure with typical features of the sulfa drug hypersensitivity syndrome occurred in a child treated for leprosy [212]. Sulfonamide hepatotoxicity results from elaboration of an electrophilic toxic metabolite in the liver. The reactive species appears to be derived from the hydroxylamine metabolite of the particular sulfonamide [213,214]. A certain proportion of patients, estimated at 11ͳ0%, develop elevated serum aminotransferases usually within a short time of starting treatment. This is a dose-responsive biochemical abnormality that resolves when the dose of valproic acid is decreased. It may be an example of "adaptation" where compensatory metabolic or biotransformation mechanisms take over and mitigate the hepatotoxic effect. Much more rarely, patients develop progressive liver failure that may resemble Reye syndrome clinically [216]. This severe form of hepatotoxicity usually does not improve when the drug is withdrawn and is frequently fatal in children [217,218]. It cannot be predicted by regular monitoring of serum aminotransferases and other liver function tests. The time from initiating treatment with valproic acid and onset of liver disease is usually less than 4 months, but longer duration of treatment does not preclude hepatotoxicity. Specific risk factors in children include age under 2 years, multiple anticonvulsant treatment along with valproic acid, coexistent medical problems such as mental retardation, developmental delay, or congenital abnormalities. Valproic acid appears to alter medium-chain fatty acid metabolism by mitochondria in an age-dependent fashion [219]. Hyperammonemia, not associated with liver failure, is another adverse metabolic effect; it is rarely associated with encephalopathy [220,221] but it mandates stopping valproic acid treatment. The severe hepatotoxicity typically presents with a hepatitis-like prodrome, mainly malaise, anorexia, nausea, and vomiting. A noteworthy feature is that seizure control may deteriorate over the same time period. Coagulopathy is often present early; jaundice typically develops later, along with other signs of progressive hepatic insufficiency such as ascites and hypoglycemia. One child with valproic acidinduced acute liver failure also had an unusual skin eruption (lichenoid dermatitis). Liver histology reviewed in one large series [217] showed hepatocellular necrosis, which may be zonal, with outright loss of hepatocytes and moribund hepatocytes remaining. Acidophilic bodies, ballooned hepatocytes, and small duct reaction may be present. Microvesicular steatosis is the most common finding overall and is often present in addition to features of cell necrosis. Hepatocellular mitochondria may be sufficiently prominent on light microscopy to make hepatocytes look granular and excessively eosinophilic. In patients presenting clinically like Reye syndrome, fever, coagulopathy, progressive loss of consciousness, severe acidosis, and variably abnormal aminotransferases are present, but the patient is not jaundiced.
However erectile dysfunction urinary tract infection order silagra 100 mg without prescription, even today, in what has been called the genomic era, specific training in metabolic genetic diseases receives marginal coverage in the curriculum of medical students and pediatric residents at many academic institutions. This situation is disconcerting because newborns and infants Liver Disease in Children, Fourth Edition, ed. The aim of this chapter is to emphasize that a methodical use of routine laboratory tests supplemented by one or two specialized investigations should allow a prompt biochemical diagnosis of patients affected with one of these metabolic diseases, preventing serious sequelae or almost inevitable death. Although effective treatment for many metabolic disorders remains unavailable or unaffordable in terms of financial requirements, ample evidence has demonstrated that a growing number of these diseases can be treated effectively and efficiently [3]. Therefore, high morbidity and mortality should not be systematically assumed in reference to these inborn errors of intermediate metabolism. Recognition of a diagnostic pattern, potentially within hours from the time of admission, may allow the implementation of adequate therapeutic measures pending confirmation of the preliminary diagnosis by specialized laboratory investigations [2]. Although blood gases, electrolytes, and glucose are routinely part of the evaluation of any acutely ill child, ammonia, lactate, and pyruvate are not consistently requested at admission. In urine, the qualitative determination of 3-keto acids by a commercial dip strip. Chemstrip; Roche Diagnostics, Basel, Switzerland) and 2-keto acids by the dinitrophenylhydrazine test can be performed at bedside in the early stage of evaluation of an acutely ill patient. A guideline for diagnostic orientation by routine laboratory investigations is shown in Table 24. Obviously, partial deviations from a model pattern are always possible, in light of the variable nature of a particular metabolic block, and the role that environmental factors play in individual patients. Other simple manual tests that could aid the differential diagnosis of other disorders in acutely ill patients include the detection in urine of reducing substances and sulfites. Gross galactosuria, however, also may occur in patients with severe liver disease of any origin, and false negative reactions for reducing substances have been observed in symptomatic newborns with galactosemia [5]. For a better understanding of the diagnostic process generally pertinent to these and other conditions, a brief recapitulation of the cardinal clinical findings of these disorders is necessary to put the laboratory analyses to be described in a practical perspective. Although the final diagnosis of a specific inborn error of metabolism is a laboratory process, several clinical elements should effectively raise the level of suspicion in that diagnostic direction. Saudubray [4] delineated several pathophysiologic patterns of clinical presentation, the recognition of which may provide valuable diagnostic signs. The clinical picture in a newborn or infant that is dominated by severe neurologic deterioration is more informative than might be assumed from the notion that limited, stereotyped responses are evoked by several different causes (sepsis, encephalitis, ingestion, Reye syndrome, and others). In the neonatal period, a patient who becomes rapidly comatose after a variable (hours to days) symptom-free period could be clinically categorized as being in an intoxication-type of neurologic distress. By comparison, the absence of a symptom-free period associated with a delayed evolution of coma is rather indicative of an energy-deficit type of neurologic distress. Specialized laboratory investigations On admission, special consideration should be given to the immediate collection and proper storage of urine and blood samples from patients in severe decompensation. These samples may not be available postmortem, or material collected even after a partial recovery may not show certain diagnostic abnormalities otherwise detectable, or more easily detectable, under acute conditions. Any volume of urine (stored at Ͳ0у with no preservatives, or even a wet diaper obtained at the emergency room) and plasma/serum (0. Alternatively, a blood spot on filter paper could provide enough material for one or more of the specialized laboratory investigations described later in this chapter. In case of death, collection of body fluids and tissues should be secured according to available protocols [7]. Quantitative profiling of amino acids, carnitine, and acylcarnitines in plasma, as well as urine organic acids and acylglycines, is the analysis of choice to reach a biochemical diagnosis for the vast majority of these disorders. There are, of course, indications, advantages, and limitations to these tests in the differential diagnosis of each group of inborn errors of metabolism. Furthermore, the provision of a detailed interpretation is essential [8], because a biochemical genetics service differs from a conventional clinical chemistry laboratory in the expectation to provide an overview of abnormal and relative negative results. Organic acidurias are a biochemically heterogeneous group of inborn errors of metabolism biochemically characterized by the accumulation of metabolites that either are not present under physiologic conditions (formed from activation of alternative pathways in response to the loss of function of a specific gene product) or are pathologic amounts of normal metabolites [9].
In the Onchocerciasis Control Programme erectile dysfunction foundation purchase silagra 100mg overnight delivery, economic gains included the agricultural benefits derived from freeing up river valleys previously not habitable due to the high risk of blindness, with an estimated 25 million hectares of land becoming available for cultivation. These diseases have a serious impact of individuals, families (as carers) and communities. They impact on the quality of life and cause loss of productivity and hence family income, inflicting a burden of cost on poor families for long-term care. This can drive people who are already poor into the medical poverty trap, as the family incurs direct and indirect medical costs which are often inappropriate. The unit costs depend on several factors, including the availability of donated drugs and the willingness of volunteers to play a key role in their distribution. Drug donations are available for onchocerciasis, lymphatic filariasis, trachoma, leprosy, fascioliasis, soil-transmitted helminths, schistosomiasis, and curative drugs are provided for sleeping sickness. Well- defined application processes are in place, together with monitoring and feedback, ensuring accountability of the use of the drugs through the complex route from manufacture, delivery and importation to their entry into the supply chain in the endemic country. This involves duty free importation, storage, distribution from the centre to communities including training needs at each level of the system and the need to monitor any adverse events. School-based deworming treatment also results in educational benefits including improved school attendance and improved physical growth and cognition. In addition, community-based interventions have been demonstrated to provide a platform for other health interventions such as vitamin A supplementation, provision of insecticide treated bednets and home-based management of malaria. Interventions through school-based delivery provide access to the school age population, nothwithstanding the need to reach those who are of school age but do not attend school. This raises issues of equity as mass drug distribution of safe and effective drugs covers large numbers of individuals who benefit directly and who would otherwise have no access to them. Such programmes often deliver drugs to populations who are beyond the reach of health services for example 50% of treatments for river blindness through the African Programme for Onchocerciasis Control are provided to communities more than 20 km from the nearest health centre. The effectiveness of interventions for elimination or control is demonstrated by historical success and in the progress of ongoing programmes, but also because communities have sustained their commitment to delivery without remuneration. These are the result of well-defined strategies, sustained country commitment to financing and the demonstration that rapid scaling up is possible following the establishment of proof of principle of the strategy. In addition, several of the products donated for mass drug administration for control of specific diseases such as lymphatic Additional needs through research Research needs are well defined-in particular the need for better drugs for some diseases such the human trypanosomiases and leishmaniases, as existing drugs are toxic, expensive, and difficult to transport and administer. These need to be given 376 Neglected tropical diseases been arrested in several countries where it is no longer a public health problem in Thailand, Sri Lanka (Brugia), Suriname, the Solomon Islands, Togo Trinidad and Tobago and Costa Rica. Annual treatments of ivermectin and albendazole are given in Africa where onchocerciasis is coendemic. Control of blindness and skin disease via the donated drug ivermectin (Mectizan; donated by Merck & Co. Onchocerciasis is also endemic in 6 countries in Latin America where twice yearly distribution of ivermectin has resulted in the elimination of transmission in several foci. In Africa there is evidence that annual distribution may also eliminate transmission if sustained for 15 years at 70% coverage. In Central America there is similar progress through control of Rhodnius prolixus. Transmission by blood transfusion has been substantially reduced throughout Latin America. Sustaining the advances made and maintaining an effective surveillance system are necessary whilst research for new and effective drugs continues to be a high priority to treat those infected. Programmes should also monitor drug efficacy as there is always a risk of resistance which becomes particularly important when few (if any) alternatives are available. Diagnostic and monitoring tools are also required as some diseases are difficult to diagnose clinically and need invasive procedures. As the diseases are often found in particular geographic regions there is a need to address them in a regional context due to the different epidemiology, diversity of health systems and health financing mechanisms. The situation has changed due to advocacy efforts and the realization that successful programmes can be implemented at low cost, the interventions are highly cost-effective. Many are based on the availability of donated drugs which are largely safe for mass drug distribution. It is also essential that there is a continuing commitment for health systems to conduct post intervention or control surveillance for several years to detect and prevent resurgence of disease. Purchase 100 mg silagra with amex. Forever Multi Maca helps with Erectile Dysfunction.
|