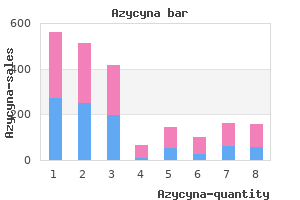
Azycyna"Buy azycyna online pills, antibiotics for sinus infection best". By: T. Cruz, M.B.A., M.B.B.S., M.H.S. Clinical Director, University of California, Irvine School of Medicine Both preparations have comparable effectiveness in the prevention of bleeding in patients with hematologic malignancy virus hives order azycyna 100mg with visa. Platelets should remain at room temperature and so are approved for only 5 days of storage because of risks of bacterial contamination and may lose viability within days after that. Prospective clinical trials are needed to better define indications for platelet transfusion and improve upon the effectiveness of transfusion therapy. Platelet transfusion therapy is associated with multiple adverse effects, including transfusion reactions, infection, alloimmunization, and immune modulation. The cost of platelets, their short storage time, and inventory pressures have made appropriate use of platelet transfusions a high priority for the management of thrombocytopenic patients to either prevent or control bleeding. Improved methods of collecting, processing, and storing platelets will be paramount in maintaining platelet inventories in the coming decade. Platelets circulate for a shorter time in thrombocytopenic patients (5 days) compared with normal subjects (8 to 10 days). Studies were performed on healthy volunteers receiving autologous radiolabeled platelets as well as on patients receiving allogeneic platelet transfusions. Data points were obtained by dividing the fixed number of platelets lost per day by the number of circulating platelets lost from turnover. Relationship between platelet count and radiolabeled platelet survival measurements in healthy and thrombocytopenic patients. The curve (solid line) was obtained from an equation predicting the dependence of platelet life span on platelet count, assuming a fixed platelet requirement. The data show a high correlation of a finite rate of random platelet destruction per day with a fixed life span of the platelets. The number of platelets needed daily to support the random loss of platelets in maintaining endothelial integrity can be calculated. For example, a man weighing 70 kg with an estimated blood volume of 5 L would need 7. To account for the platelets pooled in the spleen, an additional 30 percent should be added giving a daily requirement of 4. A somewhat higher number of platelet concentrates may be needed for patients who are also consuming transfused platelets based on clinical conditions such as sepsis, extensive tumor burden, and others. Notably, many of the patients observed in this study were treated with aspirin for pain and fever resulting in some degree of platelet dysfunction that likely increased their bleeding risk. Grade 2 bleeding, which requires some minor intervention to control bleeding, is an observable and reliable measurement for monitoring bleeding risk in platelet transfusion trials. It occurs frequently enough to be a useful end point for comparison of bleeding incidence and severity with different platelet transfusion strategies. In two large platelet transfusion trials, the incidence of Grade 2 bleeding in patients being treated for hematologic malignancies with chemotherapy was between 38 and 73 percent. In a study of 1244 hematology-oncology patients, the 198 pediatric patients had a significantly higher overall risk of Grade 2 or higher bleeding than did adults (86 percent, 88 percent, and 77 percent for patients ages 0 to 5 years, 6 to 12 years, and 13 to 18 years, respectively, vs. General Criteria for World Health Organization Bleeding Grade Categories Including Grade 2a Modification Grade 1 Minor bleeding Grade 2 Bleeding requires intervention or treatment. Hematologic malignancies accounted for approximately 9 percent of all new cancers reported in the United States in 2012. The disturbance of endothelial integrity that frequently occurs with these therapies12 and the associated inflammation can induce hemorrhage in periods of thrombocytopenia. Multiple strategies have been evaluated for maximizing the hemostatic effect of platelets while minimizing platelet use. Prospective randomized controlled trials have evaluated the relative safety of different platelet count thresholds for transfusion, whether platelets should be transfused prophylactically or can be administered therapeutically at the first sign of bleeding, and optimal platelet dose for platelet transfusion. Prophylactic platelet transfusions were shown to decrease the incidence of bleeding into vital organs noted at autopsy of leukemia patients as early as 1966,14 and have become an integral part of treatment regimens for hematologic malignancy. However, maintaining platelet counts may be difficult owing to very short platelet survivals in severely thrombocytopenic patients. Syndromes
Rendu F medication for recurrent uti generic azycyna 100 mg line, Marche P, Hovig T, et al: Abnormal phosphoinositide metabolism and protein phosphorylation in platelets from a patient with the grey platelet syndrome. Enouf J, Lebret M, Bredoux R, et al: Abnormal calcium transport into microsomes of grey platelet syndrome. Jantunen E, Hanninen A, Naukkarinen A, et al: Gray platelet syndrome with splenomegaly and signs of extramedullary hematopoiesis: A case report with review of the literature. Hirata T, Ushikubi F, Kakizuka A, et al: Two thromboxane A2 receptor isoforms in human platelets. Hirata T, Kakizuka A, Ushikubi F, et al: Arg60 to Leu mutation of the human thromboxane A2 receptor in a dominantly inherited bleeding disorder. Shiraga M, Miyata S, Kato H, et al: Impaired platelet function in a patient with P2Y12 deficiency caused by a mutation in the translation initiation codon. Cattaneo M: the platelet P2Y12 receptor for adenosine diphosphate: Congenital and drug-induced defects. Oury C, Toth-Zsamboki E, Van Geet C, et al: A natural dominant negative P2X1 receptor due to deletion of a single amino acid residue. Tamponi G, Pannocchia A, Arduino C, et al: Congenital deficiency of alpha-2adrenoceptors on human platelets: Description of two cases. Fuse I, Mito M, Hattori A, et al: Defective signal transduction induced by thromboxane A2 in a patient with a mild bleeding disorder: Impaired phospholipase C activation despite normal phospholipase A2 activation. Mitsui T: Defective signal transduction through the thromboxane A2 receptor in a patient with a mild bleeding disorder. Deficiency of the inositol 1,4,5-triphosphate formation despite normal G-protein activation. Rendu F, Breton-Gorius J, Trugnan G, et al: Studies on a new variant of the HermanskyPudlak syndrome: Qualitative, ultrastructural, and functional abnormalities of the plateletdense bodies associated with a phospholipase A defect. Malmsten C, Hamberg M, Svensson J, Samuelsson B: Physiological role of an endoperoxide in human platelets: Hemostatic defect due to platelet cyclo-oxygenase deficiency. Rak K, Boda Z: Haemostatic balance in congenital deficiency of platelet cyclo- oxygenase. Mestel F, Oetliker O, Beck E, et al: Severe bleeding associated with defective thromboxane synthetase. Lhermusier T, Chap H, Payrastre B: Platelet membrane phospholipid asymmetry: From the characterization of a scramblase activity to the identification of an essential protein mutated in Scott syndrome. Toti F, Satta N, Fressinaud E, et al: Scott syndrome, characterized by impaired transmembrane migration of procoagulant phosphatidylserine and hemorrhagic complications, is an inherited disorder. Castaman G, Yu-Feng L, Battistin E, Rodeghiero F: Characterization of a novel bleeding disorder with isolated prolonged bleeding time and deficiency of platelet microvesicle generation. Freson K, De Vos R, Wittevrognel C, et al: the 1-tubulin Q43P functional polymorphism reduces the risk of cardiovascular disease in men by modulating platelet function and structure. Berrou, E, Adam, F, Lebret, M et al: Heterogeneity of platelet functional alterations in patients with filamin A mutations. Marone G, Albini F, di Martino L, et al: the Wiskott-Aldrich syndrome: Studies of platelets, basophils and polymorphonuclear leucocytes. Moser M, Nieswandt B, Ussar S, et al: Kindlin-3 is essential for integrin activation and platelet aggregation. Breton-Gorius J, Favier R, Guichard J, et al: A new congenital dysmegakaryopoietic thrombocytopenia (Paris-Trousseau) associated with giant platelet alpha-granules and chromosome 11 deletion at 11q23. Favier R, Jondeau K, Boutard P, et al: Paris-Trousseau syndrome: Clinical, hematological, molecular data of ten new cases. Freson K, Hashimoto H, Thys C, et al: the pituitary adenylate cyclase-activating polypeptide is a physiological inhibitor of platelet activation. Sindet-Pedersen S, Ramstrom G, Bernvil S, Blomback M: Hemostatic effect of tranexamic acid mouthwash in anticoagulant-treated patients undergoing oral surgery. Siddiq S, Clark A, Mumford A: A systematic review of the management and outcomes of pregnancy in Glanzmann thrombasthenia. Peitsidis P, Datta T, Pafilis I, et al: Bernard Soulier syndrome in pregnancy: A systematic review. Nevertheless, their major clinical impact becomes apparent in the additional presence of thrombocytopenia, or additional acquired or congenital disorders of hemostasis. Acquired disorders of platelet function can be conveniently classified into those that result from drugs, hematologic diseases, and systemic disorders.
Rotunno G antibiotic cream for impetigo buy azycyna with a visa, Mannarelli C, Guglielmelli P et al; Associazione Italiana per la Ricerca sul Cancro Gruppo Italiano Malattie Mieloproliferative I. Impact of calreticulin mutations on clinical and hematological phenotype and outcome in essential thrombocythemia. Besses C, Cervantes F, Pereira A, et al: Major vascular complications in essential thrombocythemia: A study of the predictive factors in a series of 148 patients. A statement from the Italian Society of Hematology, the Italian Society of Experimental Hematology and the Italian Group for Bone Marrow Transplantation. De Stefano V, Za T, Rossi E, et al: Recurrent thrombosis in patients with polycythemia vera and essential thrombocythemia: Incidence, risk factors, and effect of treatments. Barbui T, Finazzi G: Treatment indications and choice of a platelet-lowering agent in essential thrombocythemia. Cortelazzo S, Finazzi G, Ruggeri M, et al: Hydroxyurea for patients with essential thrombocythemia and a high risk of thrombosis. Hultdin M, Sundstrom G, Wahlin A, et al: Progression of bone marrow fibrosis in patients with essential thrombocythemia and polycythemia vera during anagrelide treatment. Mohri H, Noguchi T, Kodama F, et al: Acquired von Willebrand disease due to inhibitor of human myeloma protein specific for von Willebrand factor. Pascale S, Petrucci G, Dragani A, et al: Aspirin-insensitive thromboxane biosynthesis in essential thrombocythemia is explained by accelerated renewal of the drug target. Cavalca V, Rocca B, Squellerio I, et al: In vivo prostacyclin biosynthesis and effects of different aspirin regimens in patients with essential thrombocythaemia. Landolfi R, Marchioli R, Kutti J, et al: Efficacy and safety of low-dose aspirin in polycythemia vera. Barbui T, Finazzi G: Myeloproliferative disease in pregnancy and other management issues. Foss B, Bruserud O: Platelet functions and clinical effects in acute myelogenous leukemia. Quintas-Cardama A, Han X, Kantarjian H, Cortes J: Tyrosine kinase inhibitor-induced platelet dysfunction in patients with chronic myeloid leukemia. Meschengieser S, Blanco A, Maugeri N, et al: Platelet function and intraplatelet von Willebrand factor antigen and fibrinogen in myelodysplastic syndromes. Zeidman A, Sokolover N, Fradin Z, et al: Platelet function and its clinical significance in the myelodysplastic syndromes. Frigeni M, Galli M: Childhood myelodysplastic syndrome associated with an acquired Bernard-Soulier-like platelet dysfunction. Coppola A, Tufano A, Di Capua M, Franchini M: Bleeding and thrombosis in multiple myeloma and related plasma cell disorders. Rapoport M, Yona R, Kaufman S, et al: Unusual bleeding manifestations of amyloidosis in patients with multiple myeloma. Torjemane L, Guermazi S, Ladeb S, et al: Heparin-like anticoagulant associated with multiple myeloma and neutralized with protamine sulfate. Voisin S, Hamidou M, Lefrancois A, et al: Acquired von Willebrand syndrome associated with monoclonal gammopathy: A single-center study of 36 patients. Coucke L, Marcelis L, Deeren D, et al: Lymphoplasmacytic lymphoma exposed by haemoptysis and acquired von Willebrand syndrome. Scepansky E, Othman M, Smith H: Acquired von Willebrand syndrome with a type 2B phenotype: Diagnostic and therapeutic dilemmas. Mazoyer E, Fain O, Dhote R, Laurian Y: Is rituximab effective in acquired von Willebrand syndrome Casonato A, Sponga S, Pontara E, et al: Von Willebrand factor abnormalities in aortic valve stenosis: Pathophysiology and impact on bleeding. Mitrovic M, Elezovic I, Miljic P, Suvajdzic N: Acquired von Willebrand syndrome in patients with Gaucher disease. Wiegand G, Hofbeck M, Zenker M, et al: Bleeding diathesis in Noonan syndrome: Is acquired von Willebrand syndrome the clue Mohri H, Hisanaga S, Mishima A, et al: Autoantibody inhibits binding of von Willebrand factor to glycoprotein Ib and collagen in multiple myeloma: Recognition sites present on the A1 loop and A3 domains of von Willebrand factor. Tests of platelet aggregation are abnormal in 50 to 75 percent of individuals receiving large doses (at least several grams per day) of carbenicillin antibiotics for acne minocycline buy cheap azycyna 250 mg, penicillin G, ticarcillin, ampicillin, nafcillin, and azlocillin and in 25 to 50 percent of patients taking piperacillin, azlocillin, or mezlocillin. Their effect on platelets is maximal after 1 to 3 days of administration and may remain for several days after the antibiotic has been stopped, suggesting that the effect of these antibiotics on platelets in vivo is irreversible. Although clinically significant bleeding is associated with the use of carbenicillin, penicillin G, ticarcillin, and nafcillin, it is far less common than prolongation of the bleeding time. On the other hand, high doses of penicillin G did not increase gastrointestinal blood loss in a thrombocytopenic rabbit model. A similar pattern of platelet dysfunction has been reported with some cephalosporins or related antibiotics, but not with others. Nitrofurantoin, a structurally unrelated antibiotic, may cause a mild prolongation of the bleeding time and impair platelet aggregation when blood levels of the drug are higher than 20 M, as may occur in patients with renal insufficiency. Nitroprusside can increase the bleeding time twofold when administered at infusion rates of 6 to 8 mcg/kg/min. Two preparations with average molecular weights of 40,000 and 70,000 are in clinical use. Although dextran infusions may prolong the bleeding time of normal subjects and patients with von Willebrand disease, this phenomenon has not been observed in most normal subjects. The maximal effect of dextran may require several hours, suggesting that larger molecules with a slower rate of clearance are responsible. Lower doses of hydroxyethyl starch may contribute to bleeding if administered simultaneously with low-dose heparin or if given to patients with preexistent hemostatic defects or after major cardiothoracic surgery. Antihistamines,208 the serotonin antagonist ketanserin,209 and certain radiographic contrast agents210,211 can impair platelet aggregation responses ex vivo by unknown mechanisms. For example, diets rich in fish oils containing -3 fatty acids (eicosapentaenoic acid; docosahexaenoic acid) cause a slight prolongation of the bleeding time. This is not simply the result of an elevated platelet count, because it is not encountered in reactive thrombocytosis. This includes spontaneous platelet aggregation in a patient with essential thrombocythemia and thrombosis,262 increased thromboxane biosynthesis by platelets from patients with essential thrombocythemia263 or polycythemia vera,264 and increased "procoagulant imbalance" in patients manifested by increased endogenous thrombin potential265 and increased procoagulant activity in circulating microparticles. Third, none has been prospectively shown to be predictive of bleeding or thrombosis. Fourth, although the chronic myeloproliferative neoplasms comprise several distinct clinicopathologic entities, they represent clonal abnormalities of hematopoiesis. Thrombosis also occurs in onethird of patients with myeloproliferative disorders, contributing to mortality in 15 to 40 percent of affected patients. Bleeding usually involves the skin or mucous membranes, but may also occur after surgery or trauma. Thrombosis can involve arteries or veins and may occur in unusual locations such as abdominal wall vessels or the hepatic, portal, and mesenteric circulations. Readers are referred to expert recommendations for a summary of the treatment of essential thrombocythemia and polycythemia vera, with particular relevance to risk factors for hemostasis and thrombosis (Chaps. Nevertheless, 10 to 20 percent of patients experience neurologic, gastrointestinal, and cardiac side effects, in particular fluid retention, often necessitating discontinuation of the drug. In such circumstances, 12-hour dosing may be considered, although this protocol has not been formally evaluated in a prospective clinical trial. Although aspirin was well-tolerated, there was no effect of aspirin on overall and cardiovascular mortality. Consequently, the safety and efficacy of aspirin as observed in this study may not be relevant to all patients with polycythemia vera. Pregnant women with essential thrombocythemia or polycythemia vera pose special challenges because of an apparent increased risk of unsuccessful pregnancy, thrombotic or bleeding complications, and potential teratogenicity of hydroxyurea. Purchase azycyna cheap online. CDC: 'Superbugs Out-Evolved Our Best Antibiotics'.
|