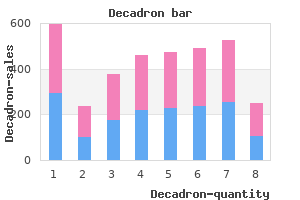
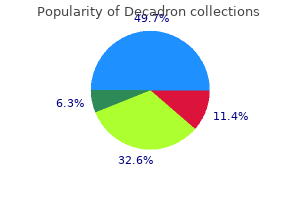
Decadron"Discount decadron 0.5 mg on-line, skin care laser clinic birmingham". By: A. Avogadro, M.A., M.D., M.P.H. Co-Director, Donald and Barbara School of Medicine at Hofstra/Northwell The same protein was also described to be a major component of Lewy bodies and Lewy neurites (see above) acne under jaw order decadron online from canada. The protein tends to aggregate as the result of a conformational change of the molecule from its unfolded, soluble form into an insoluble, b-pleated sheath. It is not clear whether aggregated -synuclein is toxic, or whether it is simply a byproduct of the disease process. The recent finding that, once initiated, -synuclein aggregation may spread to formerly healthy cells within the nervous system (Desplats et al. Early, almost universal involvement of the olfactory bulb also suggests exposure to an environmental toxin. Pathological studies have identified degeneration of nigral and locus coeruleus neurons, but Lewy bodies are not always present. Despite these shortcomings, the dopamine-depletion models of the disease are very useful for understanding the changes in brain function that are caused by dopamine loss, and for the development of symptomatic treatments for the dopaminedependent signs and symptoms of the disease. A second group of models utilizes genetically altered animals, some of which replicate abnormalities in -synuclein function. These models may be particularly useful for exploring the mechanisms of cell loss and developing neuroprotective therapies. These results indicated that striatal dopamine loss results in reduced activity in the direct pathway and increased activity in the indirect pathway, which together were thought to result in excessive activity in the basal ganglia output nuclei and greater inhibition of thalamocortical and brainstem neurons, thus leading to the hypokinetic features of parkinsonism (Albin et al. One of the obvious abnormalities is the emergence of abnormal oscillatory activity of groups of cells in the motor circuit including, the basal ganglia, thalamus and cortex in parkinsonism which may act to disrupt normal processing. In addition to oscillatory activities, the appearance of abnormal burst patterns of discharge and increased synchrony between neurons may be highly important as well. One of these consists of models that mimic the loss of dopaminergic transmission in the brain. Shown are examples of separate neurons, recorded with standard methods for extracellular electrophysiologic recording in normal and parkinsonian animals. Findings in pathologic studies may provide initial inroads to a better appreciation of the abnormalities that are responsible for some of these findings. For instance, pathologic changes in brainstem, amygdala, thalamus and cortex may contribute to dopamineunresponsive motor signs. Loss of neurons in the intermediolateral cell column of the spinal cord may be responsible, at least in part, for orthostatic hypotension, i. These treatments address the motor signs of the disease, but do not alter the course or prognosis. The oldest antiparkinsonian treatments, which are still in limited use today, are anticholinergic medications such as trihexiphenidyl and benztropine. The mechanism of action of these drugs is frequently described as a resetting of the disturbed balance between dopaminergic and cholinergic transmission in the striatum (see above). However, side effects, such as memory disturbances, blurred vision, sedation, dry mouth, and urinary retention often limit their use, particularly in older patients. The first agent to be introduced was the dopamine precursor levodopa, an amino acid that is metabolized into dopamine both peripherally and centrally. Levodopa is given in conjunction with peripherally acting blockers of the converting enzyme amino acid decarboxylase, such as carbidopa or benserazide. These reduce the gastrointestinal and autonomic side effects of levodopa and increase the availability of levodopa in the brain. Selegiline has been used for decades, whereas the more selective rasagiline was more recently introduced. These agents prolong the half-life of levodopa treatment and are used as adjunctive therapy for patients who suffer from fluctuations in their response to levodopa. Like other dopaminergic medications, levodopa therapy may induce nausea, autonomic disturbances or hallucinations. An important alternative to levodopa therapy is the use of dopamine receptor agonists such as ropinirole, pramipexole, apomorphine and rotigotine. These drugs are effective in treating parkinsonian signs, but generally do not reach the level of effect that can be achieved with levodopa treatment. Because pramipexole and ropinirole (both used in tablet form) have a longer half-life than levodopa/carbidopa, they are also useful in later stages of the disease as add-on therapy to levodopa treatment in patients whose response to levodopa/carbidopa fluctuates. Other dopamine receptor agonists (such as apomorphine) have a shorter time to onset of effect and a shorter half-life, and can be used as an injectable "rescue" treatment for patients who suffer from episodes of sudden freezing. The side effects of the dopamine receptor agonists are similar to those of levodopa, including nausea and hallucinations. Tropical sprue needs to be considered if the patient has traveled to certain geographic areas skin care home remedies purchase decadron online now, such as Asia, India, the Caribbean, and Central or South America. Malabsorptive Disorders, Small-Bowel Diseases, and Bacterial Overgrowth 97 A B of a protein-losing enteropathy. Involvement of the muscularis layer may lead to features of bowel obstruction, whereas serosal involvement may lead to ascites and peritonitis. Laboratory studies typically show an increased serum level of IgE and peripheral eosinophilia, with a more marked increase in the serum eosinophil count in patients with serosal disease. However, a normal serum eosinophil count does not exclude eosinophilic gastroenteritis. With the mucosal form of the disease, the diagnosis is established with intestinal biopsy specimens that show more than 20 to 25 eosinophils per high-power field. Parasitic infections need to be ruled out before eosinophilic gastroenteritis is diagnosed. Also, eosinophilic gastroenteritis needs to be differentiated from hypereosinophilic syndrome, which is characterized by a serum eosinophil count greater than 1. An elimination diet may be incorporated in the treatment program for eosinophilic gastroenteritis, although it has a limited role. Prednisone, 20 to 40 mg orally daily, often produces a prompt clinical response, regardless of the layer of bowel involved. Treatment with mast cell stabilizers, such as sodium cromoglycate, and leukotriene receptor antagonists, such as montelukast, has had variable success. Although budesonide can be given in place of low-dose prednisone to patients who require ongoing maintenance therapy, the controlled-release formulation of this medication may not provide adequate therapy to the proximal gastrointestinal tract. The monoclonal antibody omalizumab has provided symptomatic benefit to some patients. By comparison, in patients with chronic tropical sprue, clinical features occur gradually after several years of residence in a tropical area. Physical examination may show evidence of weight loss or cachexia, glossitis, and hyperactive bowel sounds. Laboratory features can indicate megaloblastic anemia with vitamin B12 and folate deficiency and a protein-losing state. No specific test helps establish the diagnosis, and other infectious disorders need to be ruled out. Small-bowel biopsy specimens may show villous atrophy similar to that apparent in celiac disease; therefore, for all patients with newly diagnosed celiac disease, the travel history needs to be documented, especially if the serologic test results are negative. Treatment with folate, 5 mg daily, and vitamin B12 replacement produces rapid improvement in the anemia, glossitis, and weight loss in many patients with tropical sprue. In addition, antibiotic therapy with tetracycline, 250 mg 4 times daily, may be needed in combination with folate for 3 to 6 months, especially to treat the chronic form of the disease. Primary lymphangiectasia is characterized by diffuse or localized ectasia of the enteric lymphatic system and often is diagnosed at a young age. Secondary lymphangiectasia occurs with conditions that produce impaired lymphatic flow; the causes are cardiac (congestive heart failure or constriction), neoplastic (lymphoma), or structural (retroperitoneal fibrosis). Patients present with pronounced edema, diarrhea, nausea, and vomiting; also, chylothorax and chylous ascites may be present. Laboratory findings include a decrease in the plasma level of proteins and lymphocytopenia, which may affect cellular immunity. Abnormalities of the lymphatics may also be assessed with contrast lymphangiography or nuclear scintigraphy after a high-fat load. The protein-losing state can be verified with an 1-antitrypsin clearance test (described above). Treatment of the primary form includes a low-fat, high-protein diet and supplementation with medium-chain triglycerides as needed. For the secondary form, treatment should be directed at the underlying disease process. Eosinophilic Gastroenteritis Eosinophilic gastroenteritis has various clinical manifestations depending on the location of bowel involvement. With mucosal disease, patients often have diarrhea, malabsorption, and evidence Amyloidosis Amyloidosis is a multisystem disease that frequently involves the gastrointestinal tract. Buy decadron 8mg line. MONAT SKIN.
Once the source of her bleeding is found acne 9 year old daughter buy decadron pills in toronto, decisions about admission or dismissal can be made. This pregnant patient is having nausea that is typical in the first trimester of pregnancy. Pyridoxine (vitamin B6) is a category A medication for nausea induced by pregnancy and is the first-line choice for treatment. She does not fit the criteria for hyperemesis gravidarum or require hospitalization. Heartburn is a common symptom in pregnancy and is more common in the third trimester, but patients do not have to suffer with symptoms and can be treated. There is no indication for upper endoscopy at this point since she does not have any alarm Questions and Answers 233 symptoms and has not received any treatment yet. Sodium bicarbonate can cause milk alkali syndrome and electrolyte imbalance in the fetus and is not recommended. Azathioprine was given its category D rating in the mid 1950s when it was approved to treat leukemia. In addition, by the time this patient learned that she was pregnant, organogenesis had already occurred, so that if she stopped taking the drug, she would only be putting her own health at risk. With her history of aggressive disease, monitoring alone, without use of medications, would set her up for problems if the disease flares. Mesalamine, while safe, is not appropriate treatment of Crohn disease in a patient such as this. Her disease is currently in remission, so starting a biological agent is not appropriate, nor is prescribing low-dose prednisone. Her current laboratory tests suggest that she has good graft function, and her tacrolimus level is in the therapeutic range (3-7 ng/ mL). Tacrolimus is a category C medication and is the preferred antirejection therapy when a graft is stable. In addition, there is no indication for high-dose steroids right now since her rejection episode was in the past. She has no alarm signs or symptoms to warrant endoscopy-constipation alone is not an indication for colonoscopy in a pregnant patient. Increasing dietary sources can be difficult, and thus, addition of a supplement is generally required. Castor oil is a category X therapy and should be avoided as it has been associated with uterine rupture. Magnesium citrate is low risk but only for occasional use; if the patient requires daily laxatives, docusate would be preferred. Injury of the hepatocyte membrane allows these enzymes to "leak" out of hepatocytes, and within a few hours after liver injury, the serum levels of the enzymes increase. Patients with liver disease and renal failure typically have lower levels of aminotransferases than those who have liver disease and normal renal function. Alkaline Phosphatase Alkaline phosphatase is an enzyme located on the hepatocyte membrane bordering the bile canaliculus. Because alkaline phosphatase is found also in bone and placenta, an increase in its level without other indication of liver disease should prompt further testing to discover whether the increase is from liver or from other tissues. One way of doing this is to determine the concentration of alkaline phosphatase isoenzymes. Another way is to determine the level of -glutamyltransferase, an enzyme of intrahepatic biliary canaliculi. Other than to confirm the liver origin of an increased level of alkaline phosphatase, -glutamyltransferase is of little use in the evaluation of diseases of the liver because its synthesis can be induced by many medications, thus decreasing its specificity for clinically important liver disease. Liver acid to form monoglucuronides and diglucuronides through the activity of the enzyme uridine diphosphate glucuronosyltransferase. Conjugation makes bilirubin water-soluble, allowing it to be excreted into the bile canaliculus. The serum concentration of bilirubin is measured in direct (conjugated) and indirect (unconjugated) fractions.
This patient has some relative contraindications to interferon-based therapy acne yogurt order generic decadron on line, and since she has only minimal fibrosis, there is no urgency for treatment. Discontinuation of alcohol further drives acetaminophen toward its toxic metabolites. Mildly elevated ferritin may be present with chronic alcohol use but does not suggest hereditary hemochromatosis. Ballooning degeneration and Mallory bodies are features of alcoholic hepatitis, which he does not have. Interface hepatitis with plasma cells would be seen in autoimmune hepatitis, which is less likely in this patient. The normal alpha-fetoprotein level should not dissuade you from the diagnosis, particularly in this high-risk patient. The portal vein thrombosis is due to tumor thrombus, as evidenced by arterial enhancement of the clot. Tumor thrombosis is by definition extrahepatic spread of the malignancy, so neither hepatectomy nor transplant is indicated. Anticoagulation or thrombolytic therapy does not have a role in the management of tumor thrombosis. When isolated gastric fundal varices are found, they should raise the possibility of sinistral hypertension from splenic vein thrombosis, especially in the absence of known liver disease. With a prior episode of pancreatitis, this patient has a risk factor for splenic vein thrombosis. Hepatic venography would confirm the diagnosis, but the diagnosis is fairly secure according to the constellation of clinical findings and the lack of visualization of the hepatic veins on Doppler ultrasonography. Thrombolytic therapy is used in acute hepatic vein thrombosis and should be delivered by catheter-directed therapy rather than by systemic dosing. The acute inflammatory state due to her diverticulitis is the precipitating factor. Patients with acute portal vein thrombosis should receive anticoagulation therapy to prevent progression of thrombosis and the development of portal hypertension. In the presence of an intra-abdominal inflammatory process, a bone marrow examination for hematologic disorders is not necessary. Systemic thrombolytic therapy is also not recommended in the absence of acute hepatic decompensation. Colonoscopy is relatively contraindicated in the presence of acute diverticulitis. Band ligation is not effective for large fundic varices (because of the submucosal location of the varices). Surgical expertise for splenorenal shunting typically requires transfer to a tertiary referral center and is best suited for nonemergent situations. While this patient will ultimately benefit from transplant, controlling the active hemorrhage requires emergent treatment. This patient with known cirrhosis presented with an acute upper gastrointestinal tract hemorrhage. Small esophageal varices were noted on examination, and there was evidence of recent bleeding (heme staining in the stomach). Since no other bleeding lesions were identified, the varices are the likely source and should be treated endoscopically to prevent rebleeding. While nonselective -blockade would be appropriate as part of long-term secondary prophylaxis, it does not replace endoscopic therapy, particularly in an acute bleeding episode. This patient will ultimately benefit from transplant, but controlling the active hemorrhage requires emergent treatment. This patient presents with chronic gastrointestinal tract bleeding in the presence of cirrhosis. This patient is having unacceptable adverse effects from the -blocker therapy being used as primary prophylaxis. Given his large varices, his therapy should be changed to an alternate form of primary prophylaxis-in this case, band ligation. Dose reduction may improve his symptoms, but the -blockade would likely be inadequate to prevent variceal hemorrhage (goal heart rate, about 60 beats per minute).
|