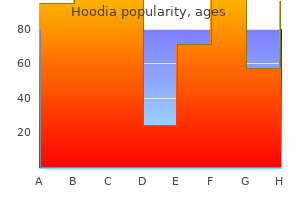
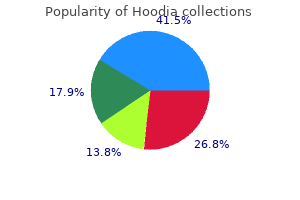
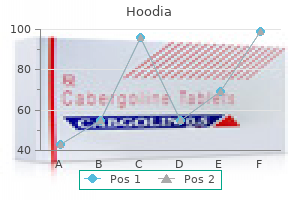
Hoodia"Generic hoodia 400mg with mastercard, herbals to lower blood pressure". By: P. Ronar, M.B. B.A.O., M.B.B.Ch., Ph.D. Professor, Northeast Ohio Medical University College of Medicine The depth of the graft site is measured from the dorsal cortex to the ventral cortex along the midline of the vertebral body herbalshopcom purchase hoodia 400 mg on-line. The length of the graft site is measured with the vertebral bodies maximally distracted and is the distance between the end plates. Gentle distraction across the corpectomy defect, using pin distractors, facilitates the strut graft placement following the corpectomy. Slight distraction across the corpectomy enables placement of a slightly larger strut graft by increasing the size of the defect, which upon release of the distraction pins will seat the graft under compression. Distraction following anterior release results in a relative reduction of the kyphosis through realignment of the vertebral bodies in plane with the distraction. The width of the planned cage also needs to be properly planned to ensure that an optimal footprint is achieved. If an interbody cage is to be placed, prior to insertion, the cages are sized with a caliper and filled with iliac crest, local autograft, or morselized allograft. With the vertebral bodies distracted, the graft is gently placed into position and should fit without excessive force or hammering. Tactile inspection of the final position of the graft should be done using a blunt hook alongside the graft. However, care should be taken to avoid spinal canal compromise or compression of neural structures by these smaller pieces of bone. If an expandable cage is to be used, the proper-sized footplates are attached to the cage. With the cage in place, the device is expanded to ensure a snug fit, taking care not to over-distract the disk space to preserve the integrity of the bony end plates. Some authors attempt to pack additional bone into the cage after it is expanded; however, it is not clear whether this can be successfully accomplished to effectively "load" the graft material within the cage. As a result, we tend to reserve the use of expandable cages for cases where a fusion might not be absolutely necessary for the success of the surgical procedure (such as with malignant tumors). A 6-mm-diameter hole is made in the center of the tubing with a rongeur, and three small holes are made laterally, two at the rostral end and one at the caudal end. Small bites are also made at the ends of the tubing to allow extrusion of cement overflow. The side of the Silastic tubing facing the spinal cord is free of the central and lateral holes to avoid cement extrusion into the spinal canal. The Silastic tubing is passed into the space between two adjacent vertebral bodies at the corpectomy site and positioned so that there is no bending of the tubing that could obstruct cement flow. Posterior Stabilization A particular area of concern in patients undergoing multilevel corpectomy is early construct failure leading to graft dislodgment. The early construct failure rate dramatically increases with multilevel constructs. Long strut grafts without points of intermediate fixation create significant stresses at the ends of long corpectomy constructs and are the likely mechanism underlying the relatively high complication rates and lower fusion rates seen in series utilizing multilevel corpectomies. The combination of anterior-posterior instrumentation has been shown to be an effective means of limiting motion with long constructs and decreasing graft migration and dislodgment. Single-level anterior diskectomy and fusion at C7-T1 as well as single-level corpectomies at C7 or T1 can be successfully managed with anterior plating and a strut graft or cage, provided there is no posterior pathology or instability. The goal of circumferential stabilization is to prevent subsequent spinal instability, spinal deformity, and excessive spinal movement that may predispose to loosening and dislodgment of the spinal construct at the corpectomy site. In general, the length of the posterior instrumentation is based on the bone quality and the overall alignment of the construct. Instrumentation should not be terminated in the midthoracic curve, to minimize the risk of pulling out the screws at the end of the instrumentation construct. The shortest plate possible is chosen that will avoid contact with the adjacent disk spaces. It is important to use a drill to remove any irregularities of the ventral surface of the vertebral bodies so that the plate can sit flush against them. A greater plate-to-bone contact provides increased structural stability for this construct. Fixed-angle screws are placed to secure the inferior end of the plate to the inferior vertebral body. Although some benign astrocytomas are well circumscribed and are suitable for gross total resection herbals shampoo buy hoodia 400mg low cost, most exhibit variable infiltration into the surrounding spinal cord. This is often reflected in a gradual transition zone between the tumor and spinal cord. Thus, whereas gross total resection may be achieved in some cases, the extent of removal is uncertain and poorly defined in most cases. Furthermore, more peripheral dissection beyond what is clearly tumor tissue risks loss of neurologic function from the resection of infiltrated, yet functionally viable, spinal cord parenchyma. Specifically, a correlation between the extent of resection and tumor control has not been definitively established. Diffusely infiltrative tumors without a definite mass are biopsied, whereas gross total resection may be possible in well-circumscribed examples. Choice of Operative Approach the vast majority of intramedullary tumors are accessed through a standard laminectomy and midline myelotomy through the posterior median septum with the patient in the prone position. Minimally invasive techniques for intramedullary tumor removal have been described but are currently limited because the morbidity of these procedures resection is related to the intramedullary tumor resection, not the initial spinal exposure. More recently, lateral and ventral approaches have been described in selected patients with more ventrally located intramedullary tumors. This interface can be assessed accurately only through an adequate myelotomy, which extends over the entire rostrocaudal extent of the tumor. Ependymomas are usually symmetrically located and exhibit uniform tumor enhancement, whereas astrocytomas are associated with a more variable appearance with respect to tumor margins and enhancement patterns. Hemangioblastomas usually appear as intensely enhancing eccentric masses or nodules. There is often diffuse spinal cord enlargement that may extend a considerable distance from the tumor. A Mayfield skull clamp is used for cervical and upper thoracic lesions above the T6 level. The acquired data, however, rarely influence the surgical technique or the surgical objective. A midline incision and subperiosteal bony dissection are made, and a standard laminectomy is performed. This should extend to at least one segment above and one segment below the solid tumor component. Delayed instability rarely occurs after laminectomy for intramedullary tumor removal in adults. Oxidized cellulose (Surgicel) is generously spread over the lateral gutters to prevent contamination of the operative field with blood. The dura mater is opened in the midline and tented laterally to the muscles with sutures. The arachnoid is opened separately, and the spinal cord is inspected for any surface abnormality. Occasionally, the overlying spinal cord may be thinned or even transparent secondary to a large or eccentrically located tumor or polar cyst. Ultrasonography is useful for tumor localization and for ensuring adequate bony exposure. Rarely, an exophytic component of a benign glial tumor may extend into the subarachnoid space through a nerve root entry zone. Malignant neoplasms may replace surface spinal cord tissue or fungate through the pia into the subarachnoid space.
The posterior lon gitudinal ligament still acts as a protective barrier between the instruments and the neural structures rumi herbals chennai buy hoodia 400 mg online. Bone wax can be used to stop the bleeding from the spongy bone, and epidural bleeds can be managed with thrombin-soaked Gelfoam or FloSeal. After opening the posterior wall, the herniated disk stained blue with indigocarmine and the hypertrophied uncovertebral region can be visualized. Foraminal decompression can be achieved by undercutting the bony prominences with a rongeur, taking care not to breach the medial foraminal wall. Dominance of the vertebral artery and the distance of the transverse foramen from the uncovertebral joint should be noted preoperatively. Subperiosteal retraction of the longus coli minimizes bleeding and protects the carotid artery. The use of indigocarmine dye facilitates the approach by identifying the disk space as well as any herniated disk fragments. While using a long bur, wobbling may be encountered, so extra care should be taken to avoid untoward injury. The surgeon should attempt to follow the direction of the previously planned trajectory. Note the narrow anterior window and the wider base posteriorly, which were done to decompress the left C6-C7 foramen. Conclusion the transcorporeal tunnel approach enables the surgeon to per form a direct anterior decompression without the need for inter body fusion. Meticulous planning and a cautious approach can provide an excellent surgical outcome. Anterior microforaminotomy for treatment of cervical radiculopathy: part 1-discpreserving "functional cervical disc surgery". Microsur gical anterior cervical foraminotomy (uncoforaminotomy) for unilateral radiculopathy: clinical results of a new technique. The treatment of certain cervicalspine disor ders by anterior removal of the intervertebral disc and interbody fusion. Transcorporeal tunnel approach for unilateral cervical radiculopathy: a 2year followup review and results. Multilevel cervical fusion and its effect on disc degeneration and osteophyte formation. Modified transcorporeal anterior cervical microforaminotomy for cervical radiculopathy: a tech nical note and early results. Posterior Approach 31 Cervical Spine: Posterior Exposure Sean Christie and Janet Martin Historically, the initial operations on the cervical spine utilized a posterior approach. However, with the advent of anterior approaches and subsequent advancement of those techniques, the posterior exposure has lost some of its favor. Concerns about relatively more postoperative neck discomfort, longer hospital stays, and the development of postlaminectomy kyphosis have contributed to this trend. Nonetheless, the posterior approach is a familiar exposure to the cervical spine, and there are several pathological conditions that favor its use (Table 31. These areas are extensively vascularized, and good hemostatic control is of necessity for proper visualization; however, dissection through the ligamentum nuchae in the midline affords a plane of relative avascularity. The vertebral arteries run through the transverse foramen of the cervical vertebrae and are generally beyond the typical exposure from the posterior approach. Morphologically, the cervical vertebrae are smaller, with bifid spinous processes, generally, to the level of C6 connected by the ligamentum flavum. As a rule, the cervical vertebrae display less shingling, enabling clear visualization of the interlaminar space. Clear distinction may be made between the lamina and the lateral mass/facet joints to the level of C6. At C7, this distinction becomes somewhat less apparent due to additional muscle attachments at this level. It should be noted that the lateral mass, also known as the zygapophyseal capsule, provides a readily visible landmark for the lateral extent of dissection in a majority of cases when instrumentation is not indicated.
Progressive changes in the biochemical composition of the intervertebral disk are responsible for a change in its water content herbs collision buy cheap hoodia 400 mg on-line, which has been demonstrated to be nearly 90% in early childhood and to decrease to less than 70% by the eighth decade. As previously discussed, as the water content decreases, the ability of the nucleus pulposus to dissipate downward forces decreases, and the intradiskal pressure rises exponentially with increasing axial loading. Transmission of this biomechanical stress to the annulus fibrosus may lead to a disk bulge. The annulus fibrosus displays an eccentric structure, with its posterior portion being thinner. Thus, a breakdown in the integrity of the annulus fibrosus is more likely to occur in such posterior areas, where it is thinner and less reinforced. Such inherent differences may account for the clinical observation that thoracic disk herniations are much rarer than their cervical or lumbar counterparts. Disk Disease of the Thoracic and Thoracolumbar Spine paresis of abdominal muscles. Patients with thoracic disk also commonly present some sort of sensory impairment, ranging from dysesthesias/paresthesias (61%) to complete sensory loss. Bladder dysfunction has been reported in 24% of cases, with urgency being the most common complaint. Spasticity and hyperreflexia occur in 58% of patients, and a positive Babinski sign can observed in 55%. Interestingly, 24% of the patients motor impairment or hyperreflexia at presentation do not complain of pain or dysesthesias. Motor weakness in the lower extremity is found in 61% of patients: 72% of them presenting paraparesis, and the remaining 28% presenting monoparesis. These rarer symptoms include nausea, emesis, chest tightness, and chronic constipation. Calcifications are found in 22 to 65% of thoracic herniations15 and are associated with up to a 40% intraoperative incidence of dural tears. According to the authors, this sign is present in up to 45% of the herniated thoracic disks. Another reason to consider surgery in these patients is the potential risk of permanent damage to the spinal cord. It has been reported that radicular pain responds better to surgery than nonradiating axial thoracic pain. In the operating room, fluoroscopy should be used to confirm the correct level, before skin incision and after the exposition of the bony landmarks. Intraoperatively, identification of the precise surgical level may be challenging in the thoracic spine, and it must be considered a crucial step during surgery for thoracic disk herniations. As already mentioned, during the procedure, high-quality fluoroscopy may be of significant help, even in the presence of modern image-guidance systems, such as navigation. Basically, surgery can be performed through a posterior, posterolateral, lateral or anterior approach. The most important goal when choosing a surgical approach is to minimize manipulation of an already compromised thoracic spinal cord. Posterolateral approaches (including the transfacetary, and the transpedicular routes, as well as the costotransversectomy technique) usually are appropriate for paracentral or lateral soft thoracic herniations. Anterior approaches (involving either an open thoracotomy or thoracoscopy) are more suitable to address large, midline, or calcified disk herniations. Recent reports have described a questionable posterior transdural diskectomy,96,97 which, although feasible, raises several concerns related Treatment the natural history of asymptomatic thoracic disk herniations is relatively benign. In a mean period of 26 months (range, 14 to 36 months), no patient developed symptoms. Of the 21 small thoracic disk herniations (defined as less than 10% of spinal canal compromise), 18 showed no significant change in size, whereas three showed a significant increase in size. Of the 20 medium-sized thoracic disk herniations (10 to 20% of canal compromise), 16 showed either a small or no change in size, one showed a significant increase in size, and three showed a significant decrease in size. Of the seven large thoracic disk herniations (defined as those with more than 20% of canal compromise), three demonstrated no change in size, and four demonstrated a significant decrease in size. In addition, five new disk herniations were detected in four patients during the follow-up period. Although there have been reports of reabsorption of calcified thoracic disks associated with resolution of the clinical symptoms,53,62 some authors believe that this type of disk herniation does not usually regress and should be always treated surgically if symptomatic.
Ambulation is started immediately after surgery herbals for arthritis discount 400mg hoodia free shipping, and the patient can be discharged on the first postoperative day, after anteroposterior, open-mouth odontoid, and lateral cervical radiographs are obtained. The favored neutral lateromedial trajectory is shown as well as the 5-degree medial alternative. If this injury happens during the exposure, the injury is invariably distal to the C1 foramen transversarium, and every attempt should be made to repair the injury because the vessel is accessible. On the other hand, if the injury happens during drilling or tapping, the surgeon will note high pressure pulsatile blood exiting the drill hole, in which case the screw should be placed as described and the procedure aborted on the contralateral side. Posterior wiring and placement of a graft should complement the procedure, if possible. Though suboptimal from the biomechanical standpoint, unilateral transarticular fixation has been reported with fusion rates of upward of 90%. Both arteriovenous fistulas and pseudoaneurysms have been reported, though the best method (occlusion versus stenting) and timing (immediate versus delayed) for endovascular treatment of stable (nonbleeding) injuries is still debated. Pseudarthrosis has not been a frequent concern, given reported fusion rates of better than 95%. Mark the C2 entry point with a bur, 3 mm lateral to the lamina-articular process junction, and 2 mm cranial to the inferior articular facet. Insert the drill through the lower cervical stab incisions, in a neutral lateromedial orientation, 25 to 30 degrees cranially; aim at the C1 anterior tubercle. If a vertebral artery injury occurs, insert a screw and abort the contralateral side. C1-C2 transarticular screw fixation is a very useful technique that can be successfully employed by most spine surgeons. Most complications can be avoided with careful preoperative planning, and patients will certainly appreciate not having to wearing a halo vest postoperatively. Radiological and anatomical evaluation of the atlantoaxial transarticular screw fixation technique. Anterolateral C1-C2 transarticular fixation for atlantoaxial arthrodesis: landmarks, working area, and angles of approach. Percutaneous anterior transarticular screw fixation for atlantoaxial instability: a case series. The optimal transarticular C1-2 screw length and the location of the hypoglossal nerve. Computer-assisted C1-C2 transarticular screw fixation "Magerl technique" for atlantoaxial instability. Traumatic spondylolisthesis of the axis: a biomechanical comparison of clinically relevant anterior and posterior fusion techniques. Biomechanical assessment of bilateral C1 laminar hook and C1-2 transarticular screws and bone graft for atlantoaxial instability. Endovascular embolization of iatrogenic vertebral artery injury during anterior cervical spine surgery: report of two cases and review of the literature. Vertebral artery complications in anterior approaches to the cervical spine: report of two cases and review of literature. Vertebral artery pseudoaneurysm complicating posterior C1-2 transarticular screw fixation: case report. Risk of internal carotid artery injury during C1 screw placement: analysis of 160 computed tomography angiograms. Up to 25% of patients may have a vertebral artery course that precludes insertion of a transarticular screw on at least one side. Borne et al6 in 1984 reported perfect results in a series of 18 patients without morbidity; these authors reported that the screw trajectory is best described as "pars-pedicle. Goel and Laheri3 in 1994 first reported the C1-C2 fixation technique utilizing a screw-plate construct. The vertebral pedicle, by definition, connects structures derived from anterior ossification centers to those derived from posterior ossification centers. The pars interarticularis, as the term implies, is the osseous structure located between the two vertebral articular processes, but this term is not found in either the Latin or English versions of the Terminologia Anatomica. Order hoodia 400mg without a prescription. Himalaya Herbals-Индийская косметика||Мой БЮДЖЕТНЫЙ УХОД за ЛИЦОМ.
|