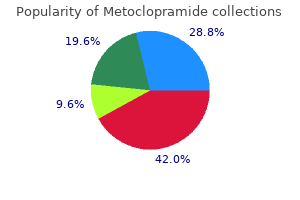
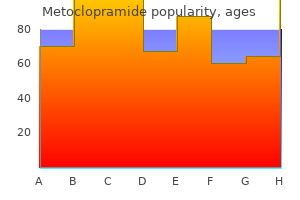
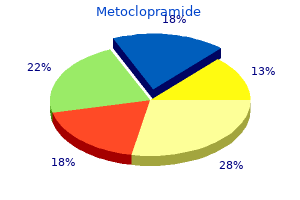
Metoclopramide"Order 10mg metoclopramide visa, gastritis vs pud". By: G. Khabir, M.B. B.CH., M.B.B.Ch., Ph.D. Co-Director, University of South Carolina School of Medicine Greenville Patch pumps have appealed to some gastritis diet 66 buy metoclopramide, as they are smaller and lighter than pumps with cannulas and are free of tubing making them more discrete. Patients require less instruction time on Insulin pumps 753 their use and the device is usually simpler in nature than the typical pump thereby reducing technical issues. A few of these pumps are already available for use; others will be in the near future [46]. The basic design comprises an insulin reservoir, delivery system and cannula, all of which are integrated into a small, wearable, disposable or semidisposable device. Other models in development allow for the handheld data manager to not only deliver insulin, but contain a glucose meter and food library. Yet another patch pump will increase the reservoir capacity so that refills occur every 6 days with the pump lasting 3 months. Next on the horizon is a closed loop completely integrated insulin delivery and glucose-sensing system. Hypoglycemia sensing remains the major concern for safety in a closed loop system. This is particularly concerning as most episodes of severe hypoglycemia happen at night [48]. This "automatic stop" function is activated when the sensor detects interstitial glucose levels below a predetermined level. Similar results were reported in the Danne study [49] in diabetic children and adolescent subjects. Reducing hypoglycemia is a central goal in the overall balance of pros and cons to any diabetes therapy. Intraperitoneal delivery of insulin has the advantage of approximating more physiologic insulin action kinetics. Intraperitoneal insulin is absorbed mainly in the portal vein, allowing for lower peripheral insulin levels and even improved glucagon response to hypoglycemia [51]. A patient using a Medtronic implantable insulin pump reported his positive experiences in 2008, offering 8 years of observations of use. With delivery of insulin directly into the peritoneal cavity, he reported feeling better, having more flexibility in eating, and fewer insulin reactions. However, at the conclusion of the article, he expresses disappointment that the manufacturer of the pump, Medtronic, no longer plans to seek Food and Drug Administration approval for this therapy [52]. The metabolic benefits, from observational studies on implantable pumps, show a decrease in HbA1c, a decrease in the frequency of severe hypoglycemia, and even less glycemic variability [45]. These benefits persist over time, even in type 1 diabetics who have not even closely reached HbA1c target of 7% and/or have large blood glucose fluctuations, severe recurrent hypoglycemia, despite tight coaching and intensified education with previous subcutaneous insulin treatment [53]. A Dutch study [54] has shown that, with an implanted insulin pump, not only was HbA1c significantly improved in those who were previously poorly controlled, but instability-related diabetic hospitalizations were also significantly reduced. However, despite reported improvement in quality of life [46], use of implantable pumps remains limited, essentially prescribed only in Europe. The limitations of this treatment mode are the result of its technically specialized medical requirements, significant cost with lack of reimbursement, as well limited manufacturing. With regard to implanted pumps coupled with glucose sensors, the pharmacokinetic properties of intraperitoneally administered insulin is of particular interest for use in a closed-loop system. Pilot studies have shown encouraging results with implanted pumps coupled with intravenous [55] and more practical subcutaneous glucose sensors [56]. Safer, smaller, smarter pumps now coupled to continuous glucose sensing have given patients a more comprehensive diabetes management tool that takes advantage of computerized programs for tracking insulin doses and integrating glucose and carbohydrate data to guide patients in improving their care. The resident intelligence of these devices has taken great strides to where they provide suggestions for bolus insulin dosing and even turn themselves Table 49. Still, no system is perfect and pumps still occlude, sensors can "break," and the transmission of data between devices can be disrupted thereby causing problems for users. As technology advances the options for diabetes management, providers must also stay in step to ensure that patients feel comfortable embracing those options. In total, the future holds much promise toward continued improvements in a system that will eventually take over the management of glucose and insulin for everyone with diabetes mellitus.
Keamseng C gastritis diet jokes discount metoclopramide 10mg fast delivery, Likitmaksul S, Kiattisathavee P: Risk of metabolic disturbance and diabetes development in Thai obese children. Lee W, Tang J, Karim H: Abnormalities of glucose tolerance in severely obese Singapore children. Boesch C, Kreis R: Observation of intramyocellular lipids by 1H-magnetic resonance spectroscopy. When hyperinsulinemia cannot compensate for exaggerated postprandial hyperglycemia, gestational diabetes develops. A new method for diagnosis of gestational diabetes mellitus has been recently suggested. Glucose crosses the placenta by facilitated diffusion during early pregnancy to supply glucose requirements of the fetus. Maternal fasting hypoglycemia may occur as a result of this enhanced glucose transport. In contrast to a seemingly normal basal insulin secretion, postprandial insulin levels are elevated, mainly due to an increase in synthesis and secretion. Insulin resistance, developing during the second half of pregnancy, is related to an elevation of several hormones, including human placental lactogen, glucocorticoids and progesterone, as well as free fatty acids and tumor necrosis factor-. Furthermore, glucose ingestion in late pregnancy results in higher and more sustained levels of glucose and insulin compared to nonpregnant subjects. Hence, it is currently possible to define better glycemic targets in order to mirror normoglycemia in pregnant diabetic women. In nonobese, nondiabetic, subjects, the difference in glucose levels between fasting and preprandial values during the day was minimal. However, mean blood glucose levels during the night-time (23:0006:00) were significantly lower than daytime levels. Hyperplasia and hypertrophy of the cells in the islets of Langerhans are ascribed to stimulation by estrogen and International Textbook of Diabetes Mellitus, Fourth Edition. They are further categorized according to length of disease and the presence of microvascular or other end-organ complications. Specifically, it has been demonstrated that approximately 67% of pregnancies in the United States are complicated by diabetes mellitus [5]. More than 90% of them are linked to maternal glucose abnormalities, especially large-for-gestational-age infants and macrosomia [6]. When other complications are considered, including spontaneous abortion, fetal malformation (principally found in pregestational diabetes), shoulder dystocia, preeclampsia, and delivery by cesarean section, the incidence of diabetes in pregnancy rises to 13%. It is estimated at up to 20% by evidence collected from high-prevalence groups, such as ethnic minorities (American Indians, Native Hawaiians and other Pacific Islanders, and Hispanics). Moreover, the offspring of diabetic mothers are at an increased risk for future insulin resistance. Thus, the major shortcoming of those criteria is the lack of correlation to adverse pregnancy outcomes. Screening and its cost-effectiveness Screening recommendations range from the inclusion of all pregnant women (universal) to the exclusion of all women except those at risk (selective). Screening policy should be determined locally, depending upon population characteristics, local prevalence and preference. A 140 mg dL-1 cutoff yields a sensitivity of nearly 90%, with a 15% positive screen rate [11]. Thus, in high-prevalence countries it is reasonable to use the lower threshold (for increased sensitivity), and the higher cut-off may be favored (for lower cost) when the prevalence is low. The test should be performed in the morning after an 814-hour overnight fast and after at least 3 days of unrestricted diet (>150 g carbohydrate per day) and physical activity. Two or more of glucose concentrations must be met or exceeded for a positive diagnosis. Caregivers and participants remained blinded to the results unless glucose values indicated overt diabetes or hypoglycemia. Hence, the rate of these complications is closely related to the degree of pregestational, periconceptional, and antenatal glycemic control. Congenital anomalies Major congenital anomalies are the primary contributor to perinatal mortality and morbidity for the offspring of a mother with pregestational diabetes, accounting for 3050% of perinatal mortality. There is a three- to fivefold increase in the incidence of congenital anomalies in infants of pregestational diabetic mothers, rising from approximately 2% incidence in the normal population to 611%. The congenital malformation rate is inversely related to maternal age at onset of diabetes and directly related to the level of glycemic control prior to pregnancy and during early pregnancy [22].
Toxic effects can be expected with as little as 20 mg/kg of elemental iron ingested gastritis like symptoms buy metoclopramide 10 mg, and doses of 60 mg/kg may be lethal. A serum iron level should be obtained, since levels between 500 and 1000 g/dL have been associated with shock and levels higher than 1000 g/dL with morbidity and mortality. If a significant amount of iron has been ingested, the patient usually presents with nausea, vomiting, and abdominal pain. Deferoxamine, an iron-specific chelator, binds free iron, creating ferrioxamine to be excreted in the urine. The intravenous route for deferoxamine is preferred, but hypotension may occur if rapid boluses are administered instead of a continuous infusion. Clinical Toxicology Lead is ubiquitous in the environment, with sources of exposure including old paint, drinking water, industrial pollution, food, and contaminated dust. However, with the elimination of tetraethyl lead in gasoline during the mid-1980s in the United States, environmental exposure to organic lead has been reduced, and most chronic exposure to lead occurs with inorganic lead salts, such as those in paint used in housing constructed prior to 1978. When lead makes its way to the bone, it impairs new bone formation and causes increased calcium deposition in long bones visible on x-ray. Lead has an apparent blood half-life of about 1 to 2 months, whereas its half-life in the bone is 20 to 30 years. Children Lead concentration in blood (ng Pb/dL) 150 Death 100 Encephalopathy Nephropathy Frank anemia Colic 50 40 30 Encephalopathy Frank anemia Adults Decreased longevity Hemoglobin synthesis Peripheral neuropathies Infertility (men) Nephropathy Systolic blood pressure (men) Hearing acuity Erythrocyte protoporphyrin (men) Hemoglobin synthesis Vitamin D metabolism Nerve conduction velocity Erythrocyte protoporphyrin Vitamin D metabolism (? Symptoms include headaches, confusion, clumsiness, insomnia, fatigue, and impaired concentration. It has been estimated that as many as 9% of the children in the United States may have blood lead levels greater than 10 g/dL. Gastrointestinal system: Early symptoms can include discomfort and constipation (and, occasionally, diarrhea), whereas higher exposures can produce painful intestinal spasms. Blood: Lead has complex effects on the constituents of blood, leading to hypochromic, microcytic anemia as a result of a shortened erythrocyte life span and disruption of heme synthesis. Elevated blood lead levels can be used diagnostically for determining lead intoxication, provided that blood lead levels are greater than about 25 g/dL. With lead levels greater than 70 g/dL or if encephalopathy is present, dual parenteral therapy is required with dimercaprol given intramuscularly and calcium disodium edetate given intravenously. Organophosphate and carbamate insecticides these insecticides exert their toxicity through inhibition of acetylcholinesterase, with subsequent accumulation of excess acetylcholine producing nicotinic (mydriasis, fasciculations, muscle weakness, hypertension) and muscarinic (diarrhea, urination, miosis, bradycardia, bronchorrhea, emesis, lacrimation, salivation) effects. Organophosphate nerve agents, such as sarin, soman, and tabun, have the same mechanism of action, but the aging process is much more rapid compared to insecticides. Atropine, a muscarinic receptor antagonist, and pralidoxime, an oxime to reactivate cholinesterase, should be administered intravenously or intramuscularly to treat the muscarinic and nicotinic effects, respectively. She also states that he has not had regular bowel movements, with mostly constipation and occasional diarrhea, and frequently complains of abdominal pain. Lead poisoning is common among children in older homes painted before lead was removed from paint. The presentation of ethylene glycol toxicity would include initial appearance of intoxication, which was not mentioned. The coworker states that the patient complained of being cold this morning around 8 am (the central heat was broken, and the outdoor temperature was 34°F) and that since noon, he had been complaining of headache, drowsiness, confusion, and nausea. Although watch makers and other professionals who use electroplating may be at higher risk for cyanide exposure because many plating baths use cyanidecontaining ingredients (for example, potassium cyanide), this patient shows signs of carbon monoxide poisoning, such as cherry red skin, headache, confusion, nausea, and drowsiness leading to unconsciousness. The history also leads us to believe that this person may have been using a space heater to stay warm, which would be consistent with the description. Cyanide in low doses from such an occupational exposure can present with loss of consciousness, flushing, headache, and confusion. Ethylene glycol and methanol toxicity may cause alterations in mental status, but the history did not include anything suggesting a toxic alcohol ingestion. Atropine is appropriate for this patient, who has symptoms consistent with organophosphate (insecticide) poisoning. An anticholinergic antidote, atropine, controls these muscarinic symptoms, whereas the antidote pralidoxime treats the nicotinic symptoms like fasciculations (involuntary muscle quivering or twitching).
In humans gastritis diet ��������� purchase 10 mg metoclopramide with amex, platelet count, activity and platelet markers all show significant diurnal variation with peak levels of activity in the morning [65] corresponding to the commonest time for myocardial infarction. In murine studies, Clock knockout is associated with abolition of diurnal variation in platelet activity and a reduction in platelet numbers to suggest an important physiologic role for Clock in the cellular phase of thrombosis [66]. Per2 knockout mice had almost 50% of normal platelet counts in the peripheral blood and showed decreased aggregation [67]. Studies of the effects of diabetes and/or obesity on circadian regulation of platelet function have not yet been reported. Insulin providers, including the sulfonylureas, have beneficial effects on glucose-mediated alterations in thrombosis; there is as yet very little information on the effects of drugs affecting the incretin system. Aspirin In addition to the antiplatelet effects, aspirin acetylates fibrinogen, altering fibrin characteristics [7072] and may influence clot lysis indirectly through a nitric oxide-dependent mechanism [73,74]. These platelet-independent fibrinolytic properties of aspirin may explain the enhanced fibrinolytic effects of streptokinase when used with aspirin [75]. Longer term, aspirin is used for secondary cardiovascular protection in diabetes [78,79], a practice supported by two large meta-analyses [80,81]. The use of aspirin for primary cardiovascular protection in diabetes is more controversial [81,82], with two recent primary prevention studies failing to show an impact of aspirin in diabetes [83,84]. In contrast, an increase in cardiovascular events was reported in aspirin-treated Chinese and Swedish diabetes subjects with no history of ischemic heart disease [86,87]. The reasons for these findings are not clear but may be related to study design (both observational and nonrandomized) and possible antiplatelet treatment of higher risk subjects. Overall, data indicate that the efficacy of aspirin in primary prevention in diabetes is compromised and should be used only in higher risk individuals. Future studies are warranted to fully categorize diabetes subjects who benefit from aspirin therapy for primary cardiovascular prevention. Clopidogrel Clopidogrel is a thienopyridine that irreversibly inhibits the platelet P2Y12 receptor. Clopidogrel is used in combination with aspirin in subjects with acute coronary syndrome and as monotherapy in those intolerant to aspirin or in patients with symptomatic cerebrovascular disease despite aspirin therapy [88,89]. However, newer agents have recently shown a superior efficacy with centers moving gradually away from clopidogrel therapy (detailed later). Prasugrel Similarly to clopidogrel, this agent irreversibly blocks the P2Y12 receptor but has a theoretical advantage through quicker metabolism and faster onset of action. However, subgroup analysis of the diabetes group showed a benefit without an increase in bleeding risk, an effect that was particularly pronounced in insulin users. This suggests that diabetes subjects have a different response to antiplatelet agents and may require different antithrombotic therapy compared with the nondiabetic population. Ticagrelol Ticagrelol blocks the platelet P2Y12 receptor; however, it differs from the thienopyridines described earlier by (i) being an active compound, (ii) reversibility of action, and (iii) shorter half-life necessitating twice daily administration. Dipyridamol and cilostazol these agents modulate the phosphodiesterase pathway to reduce platelet activation. Given the absence of an indication for dipyridamol in coronary artery disease and the questionable efficacy in cerebrovascular disease, this agent is not used frequently in clinical practice. In contrast, the use of cilostazol appears to be gaining momentum in diabetes, although large-scale studies are lacking [97,98]. However, further studies have given conflicting results in both diabetic and nondiabetic subjects, making routine use of these agents difficult to justify [100,101]. Enoxaparin is the main low molecular weight heparin used because of the predictive anticoagulative effect, ease of injections, and lower risk of thrombocytopenia. More work is needed to clarify the characteristics of individuals who would gain most benefit from this therapy. Summary and conclusions Diabetes mellitus is a chronic condition characterized by the presence of hyperglycemia and an increased risk of cardiovascular disease. Inflammatory thrombotic interactions are fundamental to the generation of vulnerable vascular lesions and to the formation of an occlusive thrombus when plaques become unstable and rupture. These interactions are sensitive to a range of metabolic abnormalities associated with both insulin resistance and hyperglycemia/glycation and the progressive nature of diabetes is tracked by progressive changes in risk for vascular damage. Thrombotic processes include the fluid and cellular phases of coagulation, fibrinolysis, and platelet function and all aspects are affected in a potentially deleterious way by diabetes and developing complications. It is important to recognize that occlusive vascular damage occurs over many years and involves a wide range of pathophysiologic processes of which thrombosis is only a part.
A comparable heterogeneous pattern of cardiac sympathetic dysinnervation has been observed in arrhythmogenic right ventricular cardiomyopathy and in patients with ventricular arrhythmias in the absence of coronary artery disease diet during gastritis order metoclopramide 10mg amex. Cardiac reflex tests assessing heart rate variation have been suggested to mainly reflect cardiac parasympathetic function. Comparisons with scintigraphically assessed sympathetic function support the view that the tests on heart variation do not absolutely differentiate between sympathetic and parasympathetic function. Cardiomyopathy Diabetic cardiomyopathy may develop independently of elevated blood pressure or coronary artery disease. This complex diabetes-associated complication is characterized by a range of molecular, structural, and functional changes (Table 73. The healthy heart is able to switch rapidly between different energy sources to adjust to different requirements. As an aerobic organ, the heart is relying to a large extent on the aerobic oxidation of substrates. The myocardial oxygen consumption is closely linked to the main determinants of systolic function, namely, heart rate, contractile state, and wall stress. In pathologic states such as heart failure or cardiomyopathy, mechanical efficiency (ratio of produced useful energy to consumed oxygen) is reduced. Fatty acyl-CoA species are able to inhibit glycolysis and are presumed to regulate Clinical features and treatment of coronary heart disease in diabetes 1069 Table 73. Myocardial capacity · Impaired diastolic compliance with normal systolic function, or no obvious functional changes. Diacylglycerol activates distinct isoforms of protein kinase C, thereby eliciting insulin resistance. A significant reduction in myocardial glucose utilization has been demonstrated in isolated diabetic cardiomyocytes and in diabetic patients. According to the Randle hypothesis, glucose accumulates in the cells and is deflected to alternate metabolic pathways, especially the pentose phosphate pathway and the hexosamine biosynthetic pathway. Oxidative stress plays a key role in the pathophysiology of diabetic cardiomyopathy. According to recent studies, the maladaptation of the heart is based on metabolic dysfunction associated with diabetes. Heart failure Type 2 diabetes and poor glycemic control have been identified as common factors influencing the incidence of heart failure. In people with diabetes, a significantly increased risk of heart failure has been demonstrated [38]. Additionally, annual mortality of diabetic patients with heart failure is increased by more than 10-fold as compared with diabetic patients without heart failure [38]. Echocardiography has been established as the preferred method for documentation of cardiac dysfunction. Echocardiography, including tissue Doppler imaging is useful in detecting myocardial dysfunction in diabetic patients, as well as in nondiabetics [4]. Measurement of plasma concentrations of natriuretic peptides or their precursors for diagnosing heart failure may also be helpful in patients with diabetes. Diastolic dysfunction is a well-established abnormality in diabetes mellitus, probably in the context of hypertension and perhaps cardiomyopathy leading to a disordered filling of the left ventricle. Quantitative and qualitative changes of the extracellular matrix formation of the heart have been observed dependent upon hyperglycemia and an excess of glucose in animal and in vitro studies and may play a role also in the human situation [28]. Echocardiographic investigations show a rapid improvement of heart muscle performance with stimulating glucose uptake by insulin administration in diabetic patients with ischemic heart disease. Blood flow and in particular reactive hyperemia induced by hypoxia may be impaired even in the absence of advanced atherosclerosis in view of profound endothelial dysfunction, and also activation, both of which seem to occur quite early on in diabetes [28]. Microvascular disease of the heart Microangiopathy represents a common and widespread manifestation in patients with multiorgan involvement. Abnormalities of coronary microcirculation have been reported in clinical diabetes mellitus using invasive or noninvasive procedures. Scintigraphic assessment, therefore, demonstrates complex patterns of dysregulation of myocardial blood flow in diabetes, which is even present in the absence of coronary artery disease. Hypoglycemia has been found to contribute significantly to increased risk of arrhythmias (see earlier and following section). Purchase cheap metoclopramide on-line. Can gastritis be cancer ? | Best and Top Health Answers.
|