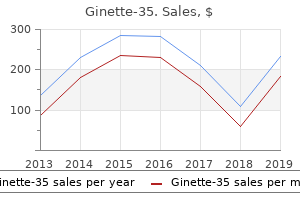
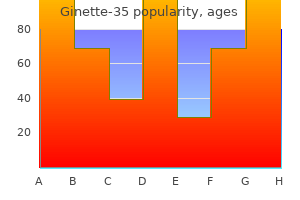
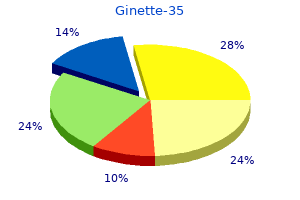
Ginette-35"Discount 2 mg ginette-35 overnight delivery, breast cancer kds". By: B. Yussuf, M.B.A., M.B.B.S., M.H.S. Clinical Director, Stanford University School of Medicine The chest radiograph can be negative early in the course womens health exam ginette-35 2 mg, or can reveal a perihilar or diffuse haziness that progresses to a finely granular, interstitial pattern. Pneumothorax with interstitial and subcutaneous emphysema and pneumomediastinum can occur. Although radiographic improvement can take several weeks, clinical improvement is usually seen within 4 to 6 days after beginning therapy. Local reactions at the injection site, tachycardia, hypotension, pruritus, hypoglycemia, and nephrotoxicity have been associated with pentamidine administration. In the United States, 1 to 3 infants per 1000 live births have Toxoplasma-specific IgM antibody. An estimated 400 to 4000 cases of congenital toxoplasmosis occur in the United States each year. Microbiology Toxoplasmosis is caused by Toxoplasma gondii, an obligate intracellular protozoan parasite. This ubiquitous organism exists in three forms: an oocyst excreted by infected cats that produces sporozoites, a proliferative form (trophozoite or tachyzoite), and a cyst (cystozoite) found in tissues of infected animals. Toxoplasma can be propagated in tissue cell cultures or by animal inoculation in research laboratories. Transmission and Pathogenesis the cat is the only definitive host, but other mammals can be infected incidentally. Farm animals (cattle, pigs, sheep) can acquire infection after ingestion of food or water contaminated with infected cat feces that contain oocysts. Humans can acquire infection by ingestion of raw or poorly cooked meat containing the Toxoplasma cysts or by ingestion of food or water contaminated with oocysts. Risk factors include any exposure to cat feces, such as changing cat litter boxes, playing in sandboxes, or gardening in areas used by cats. Congenital toxoplasmosis occurs almost exclusively as a result of primary maternal infection during pregnancy. Rarely, reactivation of infection in immunocompromised women during pregnancy can result in congenital toxoplasmosis. Fatigue and lymphadenopathy involving only a single posterior cervical node or generalized lymphadenopathy may be the only manifestation. Less commonly, acute maternal infection can manifest as an infectious mononucleosis-like syndrome with fever, nonsuppurative lymphadenopathy, headache, fatigue, sore throat, and myalgias. The general risk of transmission of acute infection from mother to fetus is estimated to be 40%; however, the actual risk and the severity of congenital infection vary with gestational age. Demonstration of Pneumocystis cysts or extracystic trophozoite forms establishes the diagnosis. It must be used with caution in young infants because of its potential for displacement of bilirubin from albumin-binding sites. The therapeutic dose is 15 to 20 mg/kg per day of the trimethoprim component in divided doses every 6 to 8 hours. The intravenous route of administration is preferable in infants with moderate or severe disease. In infants who do not respond to trimethoprim-sulfamethoxazole or in whom adverse reactions develop, pentamidine isethionate, 4 mg/kg given parenterally as a single daily dose for 14 days, can be used. Clinical Manifestations the classic clinical presentation of congenital toxoplasmosis is the triad of hydrocephalus, chorioretinitis, and intracranial calcifications, but there is a wide spectrum of manifestations, and more than 75% of infected newborns are asymptomatic in early infancy. As described by McAuley and colleagues, the four most common presentations include (1) a healthy-appearing term infant with subclinical infection in whom symptoms develop later in childhood, (2) a healthy-appearing term infant in whom clinical evidence of disease develops in the first few months of life, (3) an infant with generalized disease at birth, and (4) an infant with predominantly neurologic involvement at birth. Continued parasite proliferation may actually occur in the fetal brain despite maternal immunological control in other tissues. If the disease goes unrecognized and untreated, these infants can present with chorioretinitis, late-onset seizures, mental retardation, developmental delay, and hearing loss later in infancy or childhood. The second group of healthy-appearing, infected infants present with hydrocephalus and chorioretinitis in the first few months of life.
Cartilage-hair hypoplasia is a rare autosomal recessive disorder characterized by short-limbed dwarfism breast cancer 8mm best ginette-35 2mg, fine hair, hyperextensible digits, increased susceptibility to infection, lymphopenia, impaired cellular immunity, and chronic neutropenia. Dyskeratosis congenita is characterized by neutropenia (and other cytopenias), abnormal skin pigmentation, nail dystrophy, and mucosal leukoplakia. Other features include immunodeficiency, fragile bones, tooth decay, short stature, alopecia or premature graying, gonadal hypoplasia, urethral abnormalities, pulmonary fibrosis, liver cirrhosis, esophageal strictures, mental retardation, and a predisposition to cancers of the skin, gastrointestinal tract and other sites. Diagnosis is made by demonstration of abnormally shortened telomeres or by genetic testing, although only about half of the cases are associated with known genetic mutations. Reducedintensity hematopoietic stem cell transplantation is the only cure for patients who develop aplastic anemia. Isovaleric, methylmalonic, and propionic acidemias; hyperglycinemia; and tyrosinemia are associated with neutropenia. Congenital Neutropenia with Defective Immune System As part of the innate immune system, neutrophils participate in development of the adaptive immune system, and there are some shared receptors and proteins among lymphocytes and neutrophils. Neutropenia may be an early presenting feature of a more global and lethal immunologic defect, with or without autoimmune phenomena. Young age at presentation, failure to thrive, lymphopenia, eczema, and serious infections should be signals that a comprehensive evaluation of innate and adaptive immunity should be undertaken. Immunodeficiencies such as Bruton agammaglobulinemia, severe combined immune deficiency, DiGeorge syndrome/22q11 defects and hyperimmunoglobulin E syndrome are beyond the scope of this discussion. Griscelli syndrome type 2 shares many of these features but lacks the leucocyte inclusions. This autosomal dominantly inherited syndrome of bcl-x overexpression is characterized by severe neutropenia with myeloid hyperplasia and degraded precursor cells (myelokathexis) in the bone marrow, recurrent warts, hypogammaglobulinemia, and recurrent infections. Staphylococcal and pneumococcal infections are especially common with moderate neutropenia, which may normalize during infection. As in older children, the circulating neutrophil count increases, and a left shift occurs (band forms, myelocytes, and metamyelocytes increase in the peripheral circulation). A significant increase in early neutrophil precursors in the peripheral blood, as well as an increase in the white blood cell count (generally exceeding 50,000/), is considered a leukemoid reaction. Immature myeloid forms and even blasts can be seen in the first day or two, and these are especially common in premature infants. A leukemoid reaction associated with severe infection in the newborn often is accompanied by neutrophil cytoplasmic vacuoles and toxic granulations. Infants with Down syndrome can have a type of leukemoid reaction or even a leukoerythroblastic picture called transient abnormal myelopoiesis (see the following). Hematologic abnormalities Other Syndromes Associated with Neutropenia DownSyndrome. Infants with organ infiltration or a severe leukocytosis can be managed with low-dose chemotherapy or leukocytapheresis, respectively. Leukocyte adhesion deficiency should be suspected in any infant who has unusually severe bacterial infections accompanied by normal to increased blood leukocyte counts. There is a striking absence of pus at the site of infection because neutrophils do not migrate from the vasculature to sites of inflammation within tissues. Sialyl-Lewis X is necessary for the formation of the neutrophil cell surface ligand recognized by the endothelial cell surface E- and P-selectin receptors. Neutrophils from these patients exhibit markedly diminished chemotaxis in vitro, but have normal levels of C18. Some patients are mildly affected, whereas others develop severe, recurrent bacterial and fungal infections of skin, mucous membranes, liver, lung, spleen, and lymph nodes in the setting of increased or normal neutrophil counts. Clinical manifestations of hematologic and oncologic disorders in patients with Down syndrome. This process also sometimes occurs in a phenotypically normal child with trisomy 21 mosaicism, including an isolated clone of trisomy 21 bone marrow cells. Transient abnormal myelopoiesis is characterized by a leukoerythroblastic picture with megakaryoblasts in the peripheral blood, variable thrombocytopenia and hepatosplenomegaly. Transient myeloproliferative disorder can be life threatening or fatal from complications of hepatic fibrosis/ liver failure, hydrops fetalis, or hyperleukocytosis25 (Box 88-10). Abnormalities of polymorphonuclear leukocyte function associated with a heritable deficiency of high-molecular-weight surface glycoproteins [gP 138]: common relationship to diminished cell adherence. Chronic granulomatous disease is usually X-linked in inheritance, associated with the gp91 protein, gp91phox, but autosomal recessive forms are associated with defects in p22phox, p47phox, and p67phox. Diagnosis is made by spectrophotometric measurement of superoxide production or by measurement of reactive oxygen species production by flow cytometry, fluorometry, or chemiluminescence. Postmortem examination reveals a diffuse process womens health johnson city tn cheap ginette-35 line, with the posterior and dependent regions of the lung Treatment Several types of antimalarial drugs act at different stages of the Plasmodium life cycle. Microscopic examination reveals an eosinophilic, foamy, honeycombed intraalveolar exudate composed of cysts. In epidemic infantile disease, a plasma cellular infiltrate is observed (hence the name interstitial plasma cell pneumonia), whereas in sporadic disease associated with immunodeficiency or immunosuppression, there is hyperplasia of the cells lining the alveoli and minimal cellular infiltrate with a paucity of lymphocytes. Clinical Manifestations the clinical characteristics of sporadic Pneumocystis pneumonia are different from the characteristics observed in epidemic infantile disease. In sporadic cases associated with congenital or acquired immunodeficiency, there is an abrupt onset of high fever, coryza, nonproductive cough, and tachypnea. Concurrent infections, most commonly with cytomegalovirus, occur in more than 50% of immunocompromised infants with Pneumocystis pneumonia. In epidemic infantile Pneumocystis pneumonia, a rare disease in developed countries, the onset is slow and insidious, with nonspecific symptoms such as anorexia, diarrhea, and restlessness. In the subsequent weeks, infants become tachypneic, cyanotic, and dyspneic, with sternal retractions and flaring of the nasal alae. Auscultatory findings are minimal, consisting of fine, crepitant rales on deep inspiration. Manifestations of generalized infection at birth include prematurity and intrauterine growth restriction, jaundice, hepatosplenomegaly, pneumonitis, temperature instability, lymphadenopathy, and cutaneous lesions. Other signs of generalized infection include myocarditis; nephrotic syndrome; and gastrointestinal symptoms such as vomiting, diarrhea, or feeding difficulties. The fourth group of infected infants has predominantly neurologic disease, but can have systemic manifestations as well. Subtle neurologic deficits, obstructive hydrocephalus, or acute encephalopathy can be seen. Fetal infection is best determined using amniotic fluid polymerase chain reaction amplification of the Toxoplasma gene B1. Infection of an infant is best established definitively by intraperitoneal inoculation of placental tissue into laboratory mice, yielding cultivation of Toxoplasma organisms. When this is not feasible, strong evidence for the diagnosis is provided by the presence of Toxoplasma-specific IgM, IgA, or IgE antibody. Treatment Pyrimethamine combined with sulfadiazine and supplemented with folinic acid is recommended for treatment of symptomatic and asymptomatic congenital infection. Consultation with appropriate specialists should be sought when treating congenital toxoplasmosis. Prognosis A comprehensive maternal-fetal and infant strategy is needed to improve the outcomes of congenital toxoplasma infection. French experiences clearly show that adoption of a scheduled, monthly prenatal screening strategy decreases the transmission rate and improves the clinical outcome at the age of 3 years in the offspring. A normal outcome was documented for 100% of infants treated with pyrimethamine and sulfadiazine for 1 year when there was no evidence of substantial neurologic disease at birth. Normal neurologic or cognitive outcomes were also observed in greater than 72% of infants who did have moderate or severe neurologic disease at birth. None had sensorineural hearing loss, and most children in each group did not develop new eye lesions. These outcomes in patients treated for 1 year were markedly better than the outcomes in earlier years for infants who were untreated and infants who received only a 1-month course of therapy. There is a low but significant risk of late ocular manifestation because up to 12. Vaccine development to prevent feline oocyst shedding is ongoing, mostly with live vaccines. The Society of Obstetricians and Gynecologists has developed an excellent clinical practice guideline that is available online at sogc. Diagnosis Maternal infection occurring during gestation can lead to fetal infection. Most infants with congenital toxoplasmosis have normal results on physical examination at birth. Visual and neurologic impairment results when the infection is not diagnosed and adequately treated. Generally, all suspected maternal, fetal, and neonatal infections should have confirmatory diagnostic testing performed in an experienced reference laboratory. Buy ginette-35 without prescription. सीधी भर्ती 2018 || Female Health Worker Recruitment #Selection Process #Govt Jobs #Sarkari Naukari.
In drugs that follow zero-order kinetics menstruation or pregnancy discount 2mg ginette-35 visa, a constant amount of drug is metabolized or eliminated per unit of time regardless of concentration. There is a maximum yet constant amount that the body can eliminate at any given time. Small increases in dose can yield large increases in levels because the amount of drug removed is constant and not proportional to the dose. The elimination rate constant (Kel) is highly variable, with a smaller percentage of the drug eliminated at the beginning and a higher percentage of the residual drug eliminated toward the end. The half-life of drugs whose elimination follows zero-order kinetics is dependent on drug dosage; larger doses yield a longer half-life. The drug concentration follows a linear decrease of serum concentration over time. Phenytoin is another zero-order kinetic drug, owing to saturable kinetics of the metabolizing enzymes. The mathematical principles that describe the firstorder kinetics of the dose-to-concentration relationship over time often use a compartmental approach that best represents how a drug distributes through the body and the different rates of concentration changes in the body over time. In one-compartment models, a drug hypothetically distributes instantaneously in a homogeneous fashion into one compartment representing the entire body, and then the concentration declines linearly with one elimination rate constant (Kel) as drug is eliminated. This one-compartment approach is most appropriate for drugs that do not distribute widely into extravascular tissue. Two different exponential rates of clearance are demonstrated by a change of slope in the semi-logarithmic plot of a concentration-versus-time graph. Finally, the distribution and elimination properties of widely distributed drugs that enter and exit numerous compartments may require multi-compartment models. The mathematical principles underlying multicompartment models are beyond the scope of this chapter. The focus is on the pharmacokinetic principles that can guide clinicians in how to use therapeutic drug monitoring with only two or three plasma concentrations to determine appropriate dosing for an individual infant. This bedside pharmacokinetic approach, albeit simplified, is appropriate for many drugs used in newborns for which one- or two-compartment models are appropriate and therapeutic monitoring is available. In these scenarios, the drug concentrations at a given time after infusion are primarily impacted by the prolonged elimination beta phase. For the two-compartment model, this graph shows the immediate increase in drug in the blood followed by rapid brief alpha-phase distribution of drug followed by the slower beta phase representing metabolism and elimination. The Cmax is the maximum concentration of the drug at the end of the infusion and is used to derive the Vd. In simplest terms, the volume of distribution is the amount of drug infused divided by the amount of drug measured in the plasma. If 100 mg/kg is given and 100 mg/L is measured in the blood, then the Vd is 1 L/kg (see Table 51-1, Eq. It is important to recognize that this is an apparent volume that may exceed the physiologic blood volume because Vd takes into account the distribution of drug in the blood and peripheral tissue. When drugs are infused over prolonged time periods, then the maximal concentration of drug measured at the end of infusion may be lower than expected and may overestimate the Vd. The lower Cmax is because drug is being eliminated during the same time drug is being infused. In this case, more complicated exponential equations would be necessary to estimate the Vd while taking drug elimination into account (see Table 51-1, Eqs. Fortunately, most neonates receive drugs with short infusion times relative to the slow drug elimination rate; therefore only a very small quantity of drug is eliminated during the actual infusion, allowing the use of simplified calculations. The half-life, T1 2, is the time it takes to reduce the drug concentration [C] in half (Ln([C1]/[C2]) = Ln2 as shown in Eq. Clearance is formally defined as the volume of blood from which all drug is removed per unit of time. In practice, total body clearance is often estimated using the dose per dosing interval divided by the average steady-state drug concentration (see Table 51-1, Eq. Formulas accounting for relatively short infusions are most appropriate (see Table 51-1).
Experience with newer treatment options in young infants pregnancy 3 weeks symptoms cheap ginette-35 2mg mastercard, such as artemisinin derivatives, is limited. Severe congenital malaria can require intensive care, and exchange transfusion can be necessary for high-grade parasitemia. Current recommendations regarding treatment of congenital malaria can be obtained from the malaria branch of the Centers for Disease Control and Prevention in Atlanta, Georgia. Clinical Manifestations Most infants with congenital malaria have onset of symptoms by the eighth week of life, with an average age at onset of 10 to 28 days. Approximately one third of infants have jaundice and direct or indirect hyperbilirubinemia. Nonspecific symptoms include irritability, failure to thrive, loose stools, and reluctance to feed. Congenital malaria often is complicated by bacterial illnesses in developing countries. In rare cases, malaria can be complicated by hypoglycemia, central nervous system infection, splenic rupture, renal failure, and, in P. Microbiology Because of difficulties in laboratory cultivation, the taxonomy of Pneumocystis jiroveci (formerly Pneumocystis carinii) is inconclusive; it has features in common with protozoan parasites and fungi. Pneumocystis is a unicellular organism that can be found in three forms: a thickwalled cyst, a thin-walled trophozoite, and an intracystic sporozoite. Organisms can be detected on tissue samples stained with Grocott-Gomori methenamine silver nitrate. Diagnosis Although a maternal history of a febrile illness during pregnancy can be elicited in most cases, congenital disease after an asymptomatic pregnancy in women has been reported. The diagnosis of congenital malaria should be considered in any infant presenting with fever, anemia, and hepatosplenomegaly born to a mother who at any time resided in an endemic area. Thin and thick smears should be prepared and examined on several different occasions to maximize the possibility of parasite detection. Pathology and Pathogenesis Serologic studies suggest that asymptomatic infection with Pneumocystis is widespread and commonly occurs in the first years of life. The organisms are believed to persist in a latent stage until impairment in host defense mechanisms permits their reactivation. There is now evidence that person-to-person transmission is the most likely mode of acquiring new infections. Screening for IgG antibody in pregnancy is usually performed by indirect fluorescent antibody test or enzyme-linked immunosorbent assay and confirmed by the Sabin-Feldman dye test. Fluconazole prophylaxis in extremely low birth weight infants: association with cholestasis. Randomised controlled trial of prophylactic fluconazole versus nystatin for the prevention of fungal colonisation and invasive fungal infection in very low birth weight infants. Efficacy of fluconazole prophylaxis for prevention of invasive fungal infection in extremely low birth weight infants. Comparative virulence of Candida albicans yeast and filamentous forms in orally and intravenously inoculated mice. Cecal colonization and systemic spread of Candida albicans in mice treated with antibiotics and dexamethasone. Neonatal candidemia and end-organ damage: a critical appraisal of the literature using meta-analytic techniques. Neonatal candidiasis among extremely low birth weight infants: risk factors, mortality rates, and neurodevelopmental outcomes at 18 to 22 months. Fluconazole prophylaxis prevents invasive fungal infection in high-risk, very low birth weight infants. Infections acquired during extracorporeal membrane oxygenation in neonates, children, and adults. The control of invasive Candida infection in very low birth weight infants by reduction in the use of 3rd generation cephalosporin. Prophylactic systemic antifungal agents to prevent mortality and morbidity in very low birth weight infants. Distinctive distribution of pathogens associated with peritonitis in neonates with focal intestinal perforation compared with necrotizing enterocolitis. Safety and pharmacokinetics of multiple-dose anidulafungin in infants and neonates. Neonatal Candida meningitis: significance of cerebrospinal fluid parameters and blood cultures.
|