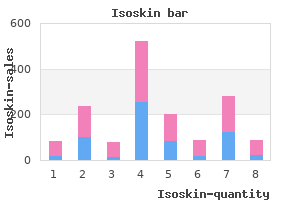
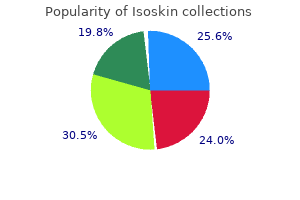
Isoskin"Buy line isoskin, acne 5 dpo". By: A. Bernado, M.B. B.CH. B.A.O., M.B.B.Ch., Ph.D. Co-Director, Stanford University School of Medicine The portion of the supracolic compartment of the peritoneal cavity immediately inferior to the liver is the subhepatic space zone stop acne generic 40 mg isoskin otc. The hepatorenal recess (hepatorenal pouch; Morison pouch) is the posterosuperior extension of the subhepatic space, lying between the right part of the visceral surface of the liver and the right kidney and suprarenal gland. The hepatorenal recess is a gravity-dependent part of the peritoneal cavity in the supine position; fluid draining from the omental bursa flows into this recess. Recall that normally all recesses of the peritoneal cavity are potential spaces only, containing just enough peritoneal fluid to lubricate the adjacent peritoneal membranes. The domed diaphragmatic surface of the liver conforms to the inferior surface of the diaphragm. This surface is divided into right and left lobes of the liver by the falciform and coronary ligaments (see also D). The peritoneal reflections (ligaments) and cavity related to the liver are shown diagrammatically. In the anatomical position, the visceral surface of the liver is directed inferiorly, posteriorly, and to the left. In embalmed 1158 specimens, impressions remain where this surface is contacted by adjacent structures. The two layers of peritoneum forming the falciform ligament separate over the superior aspect of the liver to form the anterior layer of the coronary ligament, leaving the bare area of the liver without a peritoneal covering. Of the two gravity-dependent recesses of the abdominopelvic cavity in the supine position, the hepatorenal recess is the upper one, receiving drainage from the omental bursa and upper abdominal (supracolic) portions of the greater sac. The diaphragmatic surface of the liver is covered with visceral peritoneum, except posteriorly in the bare area of the liver. The bare area is demarcated by the reflection of peritoneum from the diaphragm to it as the anterior (upper) and posterior (lower) layers of the coronary ligament. These layers meet on the right to form the right triangular ligament and diverge toward the left to enclose the triangular bare area. The anterior layer of the coronary ligament is continuous on the left with the right layer of the falciform ligament, and the posterior layer is continuous with the right layer of the lesser omentum. Near the apex (the left extremity) of the wedge-shaped liver, the anterior and posterior layers of the left part of the coronary ligament meet to form the left triangular ligament. In contrast to the smooth diaphragmatic surface, the visceral surface bears multiple fissures and impressions from contact with other organs. The four anatomical lobes of the liver are defined by external features (peritoneal reflections and fissures). Two sagittally oriented fissures, linked centrally by the transverse porta hepatis, form the letter H on the visceral surface. The right sagittal fissure is the continuous groove formed anteriorly by the fossa for the gallbladder and posteriorly by the groove for the vena cava. The umbilical (left sagittal) fissure is the continuous groove formed anteriorly by the fissure for the round ligament and posteriorly by the fissure for the ligamentum venosum. The round ligament and small para-umbilical veins course in the free edge of the falciform ligament. The lesser omentum, enclosing the portal triad (bile duct, hepatic artery, and hepatic portal vein), passes from the liver to the lesser curvature of the stomach and the first 2 cm of the superior part of the duodenum. The thick, free edge of the lesser omentum extends between the porta hepatis and the duodenum (the hepatoduodenal ligament) and encloses the structures that pass through the porta hepatis. The sheet-like remainder of the lesser omen tum, the hepatogastric ligament, extends between the groove for the ligamentum venosum and the lesser curvature of the stomach. Relationships of the liver to other abdominal viscera, lesser omentum, and portal triad. The anterior sagittal cut through the liver is made in the plane of the fossa for the gallbladder, and the posterior sagittal cut is in the plane of the fissure for the ligamentum venosum. These cuts have been joined by a narrow coronal cut in the plane of the porta hepatis. The relationship of the liver to the anterior (intraperitoneal) abdominal viscera is demonstrated. The portal triad passes between the layers of the hepatoduodenal ligament to enter the 1162 liver at the porta hepatis. Thus acne kit cheap isoskin 20 mg with visa, the descending colon of the adult can be freed from the posterior body wall (surgically mobilized) by incising the peritoneum along the lateral border of the descending colon and then bluntly dissecting along the plane of the fusion fascia, elevating the neurovascular structures from the posterior body wall until the midline is reached. Several parts of the gastrointestinal tract and associated organs become secondarily retroperitoneal. However, the roots of the short mesenteries do not arise from the midline but shift to the left or right by a fusion process like that described for the descending colon. Some of the facts relating to this include the following: the peritoneal cavity houses a great length of gut, most of which is covered with peritoneum. Extensive continuities are required between the parietal and visceral peritoneum to convey the necessary neurovascular structures from the body wall to the viscera. Various terms are used to describe the parts of the peritoneum that connect organs with other organs, or to the abdominal wall, and the compartments and recesses that are formed as a consequence. A mesentery is a double layer of peritoneum that occurs as a result of the invagination of the peritoneum by an organ and constitutes a continuity of the visceral and parietal peritoneum. It provides a means for neurovascular communications between the organ and the body wall. In this opened peritoneal cavity, parts of the greater omentum, transverse colon, and the small intestine and its mesentery have been cut away to reveal deep structures and the layers of the mesenteric structures. The mesentery of the jejunum and ileum (small intestine) and sigmoid mesocolon have been cut close to their parietal attachments. This median section of the abdominopelvic cavity of a male shows the relationships of the peritoneal attachments. The greater omentum is shown in its "normal" position, covering most of the abdominal viscera. The greater omentum has been removed from the greater curvature of the stomach and transverse colon to reveal the intestines. The greater omentum has been reflected superiorly, and the small intestine has been retracted to the right side to reveal the mesentery of the small intestine and the transverse mesocolon. The small intestine mesentery is usually referred to simply as "the mesentery"; however, mesenteries related to other specific parts of the alimentary tract are named accordingly-for example, the transverse and sigmoid mesocolons. Mesenteries have a core of connective tissue containing blood and lymphatic vessels, nerves, lymph nodes, and fat. An omentum is a double-layered extension or fold of peritoneum that passes from the stomach and proximal part of the duodenum to adjacent organs in the abdominal cavity. The greater omentum is a prominent, four-layered peritoneal fold that hangs down like an apron from the greater curvature of the stomach and the proximal part of the duodenum. After descending, it folds back and attaches to the anterior surface of the transverse colon and its mesentery. The lesser omentum is a much smaller, double-layered peritoneal fold that connects the lesser curvature of the stomach and the proximal part of the duodenum to the liver. It also connects the stomach to a triad of structures that run between the duodenum and liver in the free edge of the lesser omentum. A peritoneal ligament consists of a double layer of peritoneum that connects an organ with another organ or to the abdominal wall. The central part of the greater omentum has been cut out to show its relation to the transverse colon and mesocolon. The term greater omentum is often used as a synonym for the gastrocolic ligament, but it actually also includes the gastrosplenic and gastrophrenic ligaments, all of which have a continuous attachment to the greater curvature of the stomach. The hepatoduodenal ligament (free edge of lesser omentum) conveys the portal triad: hepatic artery, bile duct, and portal vein. The hepatogastric and hepatoduodenal ligaments are continuous parts of the 1053 lesser omentum and are separated only for descriptive convenience. The stomach is connected to the: inferior surface of the diaphragm by the gastrophrenic ligament. All these structures have a continuous attachment along the greater curvature of the stomach and are all part of the greater omentum, separated only for descriptive purposes. Isoskin 5 mg for sale. Star Hunt Online Exclusives: Get to know more about Sky's talents.
The bursa of the obturator internus allows free movement of the muscle over the posterior border of the ischium skin care vancouver isoskin 30mg free shipping, where the border forms the lesser sciatic notch and the trochlea over which the tendon glides as it turns. True to its name, the quadratus femoris is a rectangular muscle that is a strong lateral rotator of the thigh. However, it functions as a lateral rotator of the thigh, and its distal attachment is visible only during dissection of the gluteal region. The belly of the obturator externus lies deep in the proximal thigh, with its tendon passing inferior to the neck of the femur and deep to the quadratus femoris, on the way to its attachment to the trochanteric fossa of the femur. The obturator externus, with other short muscles around the hip joint, stabilizes the head of the femur in the acetabulum. It is most effective as a lateral rotator of the thigh when the hip joint is flexed. The three compartments of the thigh are demonstrated in different shades of color. Kucharczyk, Chair of Medical Imaging, Faculty of Medicine, University of 1670 Toronto and Clinical Director of the Tri-Hospital Resonance Centre, Toronto, Ontario, Canada. Thus, they span and act on two joints, producing extension at the hip joint and flexion at the knee joint. The long head of the biceps femoris meets all these conditions, but the short head of the biceps, the fourth muscle of the posterior compartment, fails to meet any of them. The hamstrings received their name because it is common to tie hams (pork thighs) up for curing and/or smoking using the long tendons of these muscles. This also explains the expression "hamstringing the enemy" by slashing these tendons lateral and medial to the knees. Full flexion of the knee requires so much shortening of the hamstrings that they cannot provide the additional contraction that would be necessary for simultaneous full extension of the thigh. Similarly, full extension of the hip shortens the hamstrings so they cannot further contract to act fully on the knee. When the thighs and legs are fixed, the hamstrings can help extend the trunk at the hip joint. The hamstrings are active in thigh extension under all situations except full flexion of the knee, including maintenance of the relaxed standing posture (standing at ease). A person with paralyzed hamstrings tends to fall forward because the gluteus maximus muscles cannot maintain the necessary muscle tone to stand straight. The hamstrings are the hip extensors involved in walking on flat ground, when the gluteus maximus demonstrates minimal activity. However, rather than producing either hip extension or knee flexion per se during normal walking, the hamstrings demonstrate most activity when they are eccentrically contracting, resisting (decelerating) hip flexion and knee extension during terminal swing (between midswing and heel strike). The length of the hamstrings varies, but this is usually a matter of 1671 conditioning. In some people, they are not long enough to allow them to touch their toes when the knees are extended. Normally, these muscles-especially their tendons on each side of the popliteal fossa-should be prominent as they bend the knee. It has a fusiform belly that is usually interrupted by a tendinous intersection and a long, cord-like tendon that begins approximately two thirds of the way down the thigh. Distally, the tendon attaches to the medial surface of the superior part of the tibia as part of the pes anserinus formation in conjunction with the tendinous insertions of the sartorius and gracilis. The tendon of the semimembranosus forms around the middle of the thigh and descends to the posterior part of the medial condyle of the tibia. The semimembranosus tendon divides distally into three parts: (1) a direct attachment to the posterior aspect of the medial tibial condyle, (2) a part that blends with the popliteal fascia, and (3) a reflected part that reinforces the intercondylar part of the joint capsule of the knee as the oblique popliteal ligament. The two medial hamstrings are not as active as the lateral hamstring, the biceps femoris, which is the "workhorse" of extension at the hip (Hamill and Knutzen, 2014). In the inferior part of the thigh, the long head becomes tendinous and is joined by the short head.
It may be involved occasionally in poliomyelitis ("polio skin care education discount 20 mg isoskin mastercard," a viral infantile disease) and generalized polyneuropathy, a disease affecting several peripheral nerves. The sensory and motor nuclei in the pons and medulla may be destroyed by intramedullary tumors or vascular lesions. Loss of the ability to appreciate soft tactile, thermal, or painful sensations in the face. Loss of corneal reflex (blinking in response to the cornea being touched) and the sneezing reflex (stimulated by irritants to clear the respiratory tract). Common causes of facial numbness are dental trauma, herpes zoster ophthalmicus (infection caused by a herpes virus), cranial trauma, head and neck tumors, intracranial tumors, and idiopathic trigeminal neuropathy (a nerve disease of unknown cause). This procedure is described in the clinical box "Inferior Alveolar Nerve Block" in Chapter 8, Head. Diplopia (double vision) is present in all ranges of movement of the eyeball, except on gazing to the side opposite the lesion. The motor paralysis of facial muscles involves superior and inferior parts of the face on the ipsilateral side. Consequently, forehead wrinkling is not visibly impaired because it is innervated bilaterally. Lesions between the geniculate ganglion and the origin of the chorda tympani produce the same effects as that resulting from injury near the ganglion, except that lacrimal secretion is not affected. Deafness There are two kinds of deafness (hearing loss): conductive deafness, involving the external or middle ear. Acoustic Neuroma An acoustic neuroma (neurofibroma) is a slow-growing benign tumor of the neurolemma (Schwann) cells. The tumor begins in the vestibular nerve while it is in the internal acoustic meatus. Trauma and Vertigo People with head trauma often experience headache, dizziness, vertigo, and other features of posttraumatic injury. Vertigo is a hallucination of movement involving the person or the environment (Roberts, 2016). It often involves a spinning sensation, but it may be felt as a swaying back and forth or falling. These symptoms, often accompanied by nausea and vomiting, are usually related to a peripheral vestibular nerve lesion. Taste is absent on the posterior third of the tongue, and the gag reflex is absent on the side of the lesion. The soft palate and posterior wall of the pharynx deviate to the contralateral side of the injury when the gag reflex is initiated ("curtain sign"). Glossopharyngeal Neuralgia Glossopharyngeal neuralgia (glossopharyngeal tic) is uncommon and its cause is unknown. These paroxysms (spasms or sudden attacks) of pain are often initiated by swallowing, protruding the tongue, talking, or touching the palatine tonsil (Yugrakh et al. Lesions of the superior laryngeal nerve produce anesthesia of the superior part of the larynx and paralysis of the cricothyroid muscle. Injury of a recurrent laryngeal nerve may be caused by aneurysms of the arch of the aorta and may occur during neck operations. Injury of the recurrent laryngeal nerve causes dysphonia (hoarseness or weakness of voice) because of paralysis of the vocal folds (cords). Paralysis of both recurrent laryngeal nerves causes aphonia (loss of voice) and inspiratory stridor (a harsh, high-pitched respiratory sound). Paralysis of recurrent laryngeal nerves usually results from cancer of the larynx and thyroid gland and/or from injury during surgery on the thyroid gland, neck, esophagus, heart, and lungs. Because of its longer course, lesions of the left recurrent laryngeal nerve are more common than those of the right. After some time, the tongue atrophies, making it appear shrunken and wrinkled (Russo et al. When the tongue is protruded, its apex deviates toward the paralyzed side because of the unopposed action of the genioglossus muscle on the normal side of the tongue. International Federation of Anatomical Associations/Federative International Programme on Anatomical Terminologies: Terminologia Anatomica: International Anatomical Nomenclature.
|