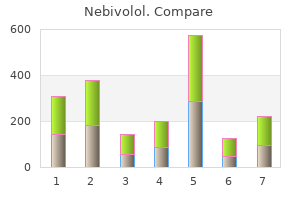
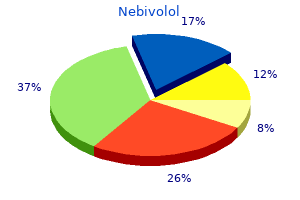
Nebivolol"Buy generic nebivolol on-line, blood pressure medication and weight gain". By: D. Mazin, M.A., M.D., Ph.D. Vice Chair, University of Toledo College of Medicine Histology shows central fibrosis of the meninges along with inflammatory cell infiltration prehypertension uk order nebivolol 5 mg with amex, which is composed mainly of lymphocytes and plasma cells, especially at the surface of the dura mater. The linear enhancement pattern appears to show better therapeutic response than the nodular form, possibly related to less fibrosis and more vascularity. Left untreated, the clinical course is usually marked by severe headaches, progressive neurologic deterioration, and visual loss. High-dose corticosteroid therapy results in improved symptoms and shrinkage of the lesions and methotrexate is an effective therapeutical option. The tumors are T1 and T2 iso- to hypointense compared to the gray matter and usually exhibit prominent contrast enhancement. In addition to sinonasal, intracranial, and intraorbital spread, the tumors may metastasize to the retropharyngeal and neck lymph nodes. Treatment with craniofacial surgery and adjuvant radiotherapy offers best outcomes. Neck dissection is performed for nodal disease, while preoperative chemotherapy is considered for large tumors. Local recurrence is not uncommon and there is a propensity for (sub) dural spread. Distant metastases may present at any time during the course of the disease, generally within 3 years, and may respond to radiation or chemotherapy. There is a bimodal age distribution with the tumors primarily involving patients in their second and sixth decades of life. Retropharyngeal lymph node metastasis from esthesioneuroblastoma: a review of the therapeutic and prognostic implications. Esthesioneuroblastoma: a case report of diffuse subdural recurrence and review of recently published studies. These tumors frequently show adjacent dural thickening, the so-called "dural tail", a nonspecific sign. Nonskull-base location, male sex, and prior surgery impart increased risk for higher grade. Vascular supply is via the meningeal external carotid artery branches, and pial vessels may be parasitized. Treatment, when necessary, is primarily surgical, with possible preoperative embolization; radiation is usually reserved for atypical and malignant tumors. Pertinent Clinical Information Meningiomas are the most frequent adult intracranial neoplasms with a predilection for women and African ethnicity. They can be clinically silent incidental findings (90%), or can cause variable signs and symptoms depending on their size and location. Most meningiomas are benign and slow-growing; some grow rapidly, which is not limited to higher-grade tumors. There is marked vasogenic edema (arrowheads) and mass effect with leftward midline shift (black arrow). Post-contrast images show marked enhancement of the solid portion along with enhancement extending to the adjacent leptomeninges and dura. Typically it shows non-enhancing walls and may appear multilobulated due to the presence of septations; areas of enhancement may at times be present within the cystic septa. Calcification and hemorrhagic foci are usually absent whereas perifocal edema is variable and often very prominent. The lesion is usually massive and replaces large portions of the affected hemisphere. The superficial solid portion primarily involves the leptomeninges and superficial cortex, and is commonly attached to the dura. Histologically, it is characterized by the presence of a prominent desmoplastic stroma, a variable amount of neuroepithelial and neuronal cells, and aggregates of poorly differentiated cells. The presence of desmoplasia (dense fibrocollagenous bands) represents a distinctive feature of these tumors and accounts for the very low signal intensity on T2-weighted images. Pertinent Clinical Information Affected infants present with asymmetric macrocrania, bulging of the fontanels and other nonspecific symptoms such as seizures and vomiting. Desmoplastic supratentorial neuroepithelial tumours of childhood: imaging in 5 patients. Her physical examination does not reveal any hernias and is consistent with that of distal small bowel obstruction blood pressure medication valsartan buy nebivolol 5 mg on line. A 45-year-old woman who has small bowel obstruction after open gallbladder surgery 20 days previously D. A 2-day-old male infant who has small bowel obstruction because of jejunal atresia E. A 20-year-old man with partial small bowel obstruction associated with an incarcerated inguinal hernia 6. The patient has anion gap acidosis as evidenced by the low bicarbonate level, which is probably caused by lactic acid, reflecting ischemic bowel or severe fluid depletion. Elderly patients, age 65 or older, often have a minimum of symptoms and are often afebrile in the face of inflammatory or infectious conditions. Laparotomy is a reasonable option, if the patient has not made any progress with conservative management. Continued nonoperative treatment without further assessment is not appropriate in this patient who is without any prohibitive risks or contraindications for surgery. Persistent pain, fever, tachycardia, leukocytosis, an elevated serum amylase level, and radiographic signs of high-grade small bowel obstruction are often signs of complicated bowel obstruction and the need for surgical therapy. She denies a history of trauma, exposure to heavy metals, or a family history of multiple sclerosis. Considerations the distribution of the progressive numbness and pain is suggestive of median nerve compression. The mechanism of this disorder is compression of the median nerve as it passes within the carpal tunnel. Median nerve compression causes numbness and pain in the thumb, index finger, and middle and lateral aspects of the ring finger. The median nerve may be compressed anywhere along its length from the brachial plexus down to the hand, but the most common site of compression is within the carpal tunnel, where it is dorsal to the transverse carpal ligament. The carpal canal is a rigid structure that causes physiologic dysfunction by producing median nerve ischemia. The best initial management is a nighttime splint for the wrist and avoidance of excess activity with the hand. The walls and floor on the dorsal surface of the canal are formed by the carpal bones, and the ventral aspect is confined by the strong, inelastic, transverse carpal ligament. Exacerbation of symptoms at night is thought to be caused by edema; tenosynovitis may also be present. Other causes are autoimmune disorders, lipomas of the canal, bone abnormalities, and hematomas. The exertion of direct digital pressure by the examiner over the median nerve at the carpal tunnel frequently reproduces the symptoms in approximately 30 seconds. In the Phalen maneuver, gravity-induced wrist flexion also produces the classic symptoms of this condition. A positive Tinel sign is present when direct percussion over the nerve reproduces paresthesia. Sensory loss, particularly vibration sense, and motor loss may be present with thenar muscle wasting and decreased abductor muscle resistance. The wrist in cross section reveals that the median nerve is susceptible to impingement. A comparison of median and ulnar or median and radial sensory stimulation values at the wrist is useful in confirming the diagnosis. Radiographs, including a "carpal tunnel view," are recommended to detect arthritis or fractures. Treatment Conservative therapy consists of the use of splints and nonsteroidal anti-inflammatory agents. Splints should be light and hold the wrist in a neutral or slightly extended position. Purchase nebivolol canada. #Promo H8 Women Female Smart Bracelet Heart Rate Blood Pressure Sleep Monitor Smart Band Fitness Tr.
The typical onset of this clinical syndrome is often insidious and marked by nonspecific symptoms of malaise hypertension uncontrolled icd 9 order 5 mg nebivolol with mastercard, headache, nausea, and confusion; it can progress rapidly to shock and death. Early medical evaluation at the first signs of illness is important in decreasing mortality. The most common organisms are encapsulated bacteria such as Streptococcus pneumoniae, Haemophilus influenzae B, and Neisseria meningitidis, which are typically killed by the immunologic functions of the spleen. All patients undergoing planned elective splenectomy should receive a polyvalent pneumococcal vaccination 2 weeks before surgery. Children and all immunosuppressed patients should be vaccinated against pneumococcus, H influenzae B, and meningococcus. Her platelet count has decreased from the initial posttreatment level of 120,000 to 75,000. The patient has remained asymptomatic without further treatment for the past 3 months. Which of the following is the most appropriate recommendation for this patient at this time Laparoscopic splenectomy because she has had a favorable but unsustainable response to steroids treatment B. Vaccination against pneumococcus, H influenzae B, and meningococcus, followed by laparoscopic splenectomy 2 weeks later E. During his exploratory laparotomy, splenic lacerations were identified and treated with a partial splenectomy. Which of the following studies may be helpful to determine if the patient has retained splenic functions following this procedure An 8-year-old boy who underwent splenectomy for complications related to acute lymphocytic leukemia 2 years prior C. A 60-year-old man with hypercoagulable state and splenic vein thrombosis and partial splenic infarct D. A 12-year-old boy with history of trauma and partial splenectomy at the age of 8 E. The presence of these peripheral smear abnormalities indicates that the absence of normal immunological functions of the spleen is not clear. Splenectomy for adult patients with idiopathic thrombocytopenic purpura: a systemic review to assess long-term platelet count responses, prediction of response, and surgical complications. He has been receiving infliximab (Remicade) infusions at 5 mg/kg every 8 weeks for the past 8 months. Before that time, he had taken prednisone 40 mg/d for several weeks intermittently for treatment of disease exacerbation. The complete blood count revealed a white blood cell count of 14,000/mm3, and his hemoglobin level is 10. The results from serum electrolyte studies and a urinalysis are within the normal range. Currently, he has nausea, vomiting, abdominal pain and distention, and a low-grade fever and leukocytosis, which are suggestive of chronic small bowel obstruction and low-grade sepsis. Exacerbations required steroid therapy in the past; however, he has now received several doses of infliximab. Obstruction from subacute inflammation can be resolved with anti-inflammatory and immunomodulator therapies. In contrast, fibrotic strictures cannot be resolved with medical management and generally require surgical therapy to relieve the obstruction. Once the small bowel and colon have been evaluated, this patient should undergo exploratory laparotomy to relieve his bowel obstruction. Histologic, endoscopic, radiographic, and surgical criteria frequently do not correlate with clinical criteria and may not correlate with the physiologic impact of the disease on the patient. Intra-abdominal Crohn disease usually results in one of three predominant disease patterns: stricture, perforation, or inflammation. The strictured segment of bowel is divided longitudinally then reapproximated transversely, thus increasing the diameter of that segment without resection. This approach may help preserve bowel length and function for patients with involvement of multiple sites by fibrotic strictures. Anorectal involvement is frequently found in patients with small bowel Crohn disease and may be the initial manifestation in 10% of patients. Therefore, Crohn disease should be considered whenever recurrent or complex perianal abscesses and fistulas are encountered. The other symptoms related to Crohn disease are often nonspecific, including chronic abdominal pain, postprandial abdominal cramps, weight loss, or fever related to fistulizing disease. It is not uncommon for patients with Crohn disease to have symptoms for months to years before the diagnosis is established.
A more subtle dark lining is present along the mesial temporal lobes and vermis (arrowheads) hypertension quotes order nebivolol discount. A black line follows the contour of the cerebellum, medulla, pons, and midbrain and to a lesser extent the supratentorial regions such as the temporal lobes (particularly the sylvian and interhemispheric fissures). The cerebellum commonly shows atrophy particularly in its vermis and the anterior aspects of the hemispheres. Chronic exposure of brain cells (particularly microglia and oligodendrocytes) to hemosiderin leads to their production of ferritin, which worsens the process. Schwann cells are particularly prone to damage, which explains frequent sensorineural hearing loss in these patients. Because the cochlea is spared, implantation may improve hearing loss in some individuals. Pyramidal signs and loss of bladder control are observed in a small number of patients and at the end of the disease, dementia will develop in about 25% of patients. The peripheral nervous system is not affected but involvement of spinal nerve roots may give rise to conflicting clinical symptoms. A more cephalad image (B) shows corrugated appearance of the affected cortex (arrowheads) and reduced sulci. High-resolution images reveal that the cortical ribbon itself is thin, and the apparent thickening results from juxtaposition of the small folds. The perisylvian cortex is the site most commonly affected by polymicrogyria; however, any region of the cortical mantle can be involved. Cortical involvement can be restricted to a single focus or it can affect extended areas, as seen in cases of uni- or bilateral, symmetrical or asymmetrical, diffuse polymicrogyria. The imaging appearances of polymicrogyric cortex can be heterogeneous, ranging from multiple abnormal small gyri to a relatively smooth cortical surface and an overall coarse appearance. Polymicrogyria may be associated with schizencephaly, corpus callosum dysgenesis, cerebellar hypoplasia, periventricular and subcortical heterotopias. An imaging protocol including volumetric T1-weighted images with thin sections (< 1. It is caused by disturbance of the late neuronal migration or early cortical organization. The deep neuronal layers do not develop normally, leading to overfolding and abnormal lamination of the cortex. The development of these irregular undulations occurs as early as 18 gestational weeks, before the first primary sulci form at midgestation. Because it is a primary cortical disorder, both connectivity and gyration/sulcation of these regions are very abnormal. In addition, the overlying meninges are thickened and may demonstrate vascular proliferation of unclear etiology. Causes of polymicrogyria include congenital infection (especially cytomegalovirus infection), mutations of one or multiple genes, and in-utero ischemia. It can also occur with several chromosomal deletion and duplication syndromes (Aicardi, DiGeorge, and Delleman syndromes, among others). Pertinent Clinical Information Clinical manifestations and the age of presentation vary depending on the location of the malformation, the extent of cortical involvement (focal, multifocal, diffuse, unilateral, or bilateral), and the presence or absence of associated anomalies. Patients affected by unilateral or bilateral diffuse polymicrogyria present with moderate or severe intellectual impairment, mixed seizure types, and motor dysfunction. Individual clinical features include hemiparesis or tetraparesis, speech disturbance, dyslexia, and developmental delay. Coexistent anomalies include dysmorphic facial features, hand, foot, skin, palate, and cardiac abnormalities. Development and dysgenesis of the cerebral cortex: malformations of cortical development. Mesial temporal lobes are typically affected but other parts of the brain may also be involved. Findings generally disappear from 2 weeks to 2 months after the ictus and the affected regions return to normal or become atrophic.
|