Tri azit"Safe 100 mg tri azit, antibiotics z pack dosage". By: K. Sobota, M.A., M.D., Ph.D. Medical Instructor, University of Oklahoma College of Medicine Ipsilateral stroke occurred in 16% of those with progression and in 9% of those with stable degree of stenosis and no strokes were seen in the patients with plaque regression (relative risk bacteria under fingernails purchase 100mg tri azit with amex, 1. The incidence of stenosis progression was inversely proportional to the degree of stenosis. Carotid endarterectomy for asymptomatic carotid stenosis: asymptomatic carotid surgery trial. Systematic review of the risks of carotid endarterectomy in relation to the clinical indication for and timing of surgery. Medical (nonsurgical) intervention alone is now best for prevention of stroke associated with asymptomatic severe carotid stenosis: results of a systematic review and analysis. Low risk of ipsilateral stroke in patients with asymptomatic carotid stenosis on best medical treatment: a prospective, population-based study. Identifying which patients with asymptomatic carotid stenosis could benefit from intervention. Absence of microemboli on transcranial doppler identifies low-risk patients with asymptomatic carotid stenosis. Effects of intensive medical therapy on microemboli and cardiovascular risk in asymptomatic carotid stenosis. Asymptomatic internal carotid artery stenosis and cerebrovascular risk stratification. Effect of image normalization on carotid plaque classification and the risk of ipsilateral hemispheric ischemic events: results from the asymptomatic carotid stenosis and risk of stroke study. Juxtaluminal hypoechoic area in ultrasonic images of carotid plaques and hemispheric symptoms. The size of juxtaluminal hypoechoic area in ultrasound images of asymptomatic carotid plaques predicts the occurrence of stroke. Composition of carotid atherosclerotic plaque is associated with cardiovascular outcome: a prognostic study. Silent embolic infarcts on computed tomography brain scans and risk of ipsilateral hemispheric events in patients with asymptomatic internal carotid artery stenosis. Predictors and clinical significance of progression or regression of asymptomatic carotid stenosis. For this reason, surgical treatment of either cerebellar hemorrhage or cerebellar infarction should be listed under the rather broader category of management of vascular-related mass effect in the posterior fossa. The hematoma thus begins in the cerebellar hemisphere, although it may extend medially to involve the vermis or the contralateral hemisphere, and therefore may dissect into the fourth ventricle, resulting in intraventricular hemorrhage [2,3]. Direct involvement of the brain stem is unusual, but brain stem compression from mass effect, as is seen in both cerebellar hemorrhage and infarction, is not only common, but is the major cause of morbidity and mortality from these conditions. Besides hypertensive hemorrhage, other etiologies of a cerebellar hematoma need to be ruled out. Patients with hereditary, acquired, or iatrogenic coagulopathies are at significantly increased risk for cerebellar hemorrhage. Underlying structural causes of hemorrhage may be present in any patient, but are most common in younger patients, in nonhypertensive patients, or in patients with hematoma localized to the cerebellar vermis. Structural causes of hemorrhage would include primary or metastatic brain tumors, vascular anomalies, sterile or septic thromboemboli and, related to the above, hemorrhagic transformation of a cerebellar infarction. A careful search for an underlying structural cause needs to be made in all patients who present atypically, according to the criteria mentioned. In our experience, a traumatic etiology for cerebellar hemorrhage (as opposed to supratentorial traumatic hemorrhage) is extremely rare and has been seen only in association with major head trauma. The exception to this rule would be patients with coagulopathies who may have either spontaneous cerebellar hemorrhage or cerebellar hemorrhage associated with very minor head trauma. The signs and symptoms of cerebellar hemorrhage are very similar to those for cerebellar infarction and, once again, relate to the resultant mass effect in the posterior fossa. Heros has outlined the following three major stages that form the hallmarks of the clinical presentation of posterior fossa mass effect [1]. In the early stage, symptoms are related to destruction of cerebellar tissue and/or extension of hematoma into the subarachnoid space. These symptoms include dizziness, nausea, vomiting, headache, balance difficulties, and gait ataxia.
In contrast there is extensive spontaneous plasticity of brain connectivity antibiotics for dogs lyme disease buy tri azit uk, in development, learning, and after injury. Harnessing therapeutic plasticity to support collateral axon sprouting and functional reconnections offers great promise for functional improvement after stroke. Advances in understanding of glial cell differentiation and development provide approaches to repopulation of oligodendrocytes [12] and replacement of lost myelin after ischemic and other white matter injuries. Understanding the complex and intertwined pathophysiological processes involved in ischemic damage of axons and glial cells is essential for long-term development of effective stroke therapies. Role of acute lesion topography in initial ischemic stroke severity and long-term functional outcomes. The ischemic penumbra: the location rather than the volume of recovery determines outcome. Ampa/kainate receptor activation mediates hypoxic oligodendrocyte death and axonal injury in cerebral white matter. Therefore antiinflammatory strategies that would seek to inhibit the direct effects of inflammation on neuronal homeostasis have been the focus of numerous neuroprotective strategies, with promising results in animal models of ischemic stroke. However, this approach has failed to translate into any measurable clinical utility, and treatment options for focal ischemic stroke remain largely limited to early reperfusion via thrombolytics or clot retrieval. One explanation for the translational failure of antiinflammatory approaches is that strategies targeting neuronal survival alone may be insufficient to result in any measurable improvement in outcome. Therefore there has been an increased interest in the roles of other cell types in the inflammatory response in the brain following thrombotic stroke. Within minutes of ischemia the cascade of regional neuroinflammatory events that occurs is mediated by the activation of local microglia and astrocytes, specialized glial cells that represent the largest proportion of cells in the mammalian brain. This chapter will discuss the critical role that microglia and astrocytes play in the induction of poststroke neuroinflammation, and their potential as targets in the next generation of therapeutic strategies for thrombotic stroke. Microglia are distributed relatively uniformly throughout the brain, although specific microglial populations may exist in different regions, depending on local biochemical features and in response to chemoattractants and inflammatory mediators released by neurons and astrocytes. The primary functions of microglia are: (1) pathogen recognition; (2) phagocytosis of damaged/apoptotic cells, small and inactive synapses, tissue debris, infectious agents, and certain macromolecules; and (3) regulation of T-cell responses and induction of inflammation. Under normal physiological conditions, microglia exist in a resting state, characterized by a ramified morphology with little cytoplasm. Although "resting," these cells are highly dynamic with continuous extension and retraction of processes that actively survey the local microenvironment. Cerebral ischemia induces microglial activation [1], characterized by a change in shape to amoeboid, loss of branching processes and production of lysosomes and phagosomes, and secretion of proinflammatory mediators. Activated amoeboid cells appear abundant in the ischemic core, whereas microglia in the penumbra remain ramified. This active state has been traditionally considered detrimental for neuronal fate, and early drug therapies targeted prevention of microglial activation. However, similar to astrocytes, activated microglia have been observed to exert both injurious and protective effects subsequent to cerebral ischemia [2]. This ambiguity has been partially resolved by the observation that microglia have the ability to transform into a range of activated states with polarization phenotypes, varying between M1 and M2 activation states. Morphologically, microglia of both M1 and M2 activation states become spherical and retract cell processes; therefore differentiation between the two states is solely Primer on Cerebrovascular Diseases, Second Edition dx. In M1 or "classical" activation, microglia are characterized by upregulation of proinflammatory surface antigens (Table 27. The protective role of these cells is thought to be mediated by their high capacity to phagocytize apoptotic and damaged cells (thereby preventing release of their cellular content into the extracellular space) and to phagocytize various potentially injurious molecules that have been already released in the extracellular space. Differentiation into the M2 phenotype can be induced in vivo by pathological events that do not cause abundant necrosis. Activation of microglia varies between M1 and M2 states, which generally have opposing effects on neuronal fate. On binding complement receptors, microglia become activated and in turn contribute to the autocrine complement cascade. Observations suggest the time course of polarization and the relative abundance of the two phenotypes depend on the severity, location, and duration of ischemia and reperfusion [1]. Microglia were previously found to produce proinflammatory cytokines and express M1 markers within the first 24 h following the onset of focal ischemia [4]. Subsequently, markers of M2 were observed in the ischemic core at 24 h, peaked after 5 days, and then declined by 14 days after ischemia, whereas the number of cells expressing the M1 phenotype gradually increased after ischemia and peaked after 2 weeks [1].
Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomized trials antibiotic for lyme disease discount generic tri azit canada. Oral anticoagulants vs aspirin in nonvalvular atrial fibrillation: an individual patient meta-analysis. Should patient characteristics influence target anticoagulation intensity for stroke prevention in nonvalvular atrial fibrillation New oral anticoagulants and the risk of intracranial hemorrhage: traditional and Bayesian meta-analysis and mixed treatment comparison of randomized trials of new oral anticoagulants in atrial fibrillation. Comparative effectiveness of warfarin and new oral anticoagulants for the management of atrial fibrillation and venous thromboembolism: a systematic review. Nonvitamin-Kantagonist oral anticoagulants in patients with atrial fibrillation and previous stroke or transient ischemic attack: a systematic review and meta-analysis of randomized controlled trials. Factor Xa inhibitors versus vitamin K antagonists for preventing cerebral or systemic embolism in patients with atrial fibrillation. Direct thrombin inhibitors versus vitamin K antagonists for preventing cerebral or systemic embolism in people with non-valvular atrial fibrillation. Indications for early aspirin use in acute ischemic stroke: a combined analysis of 40 000 randomized patients from the Chinese Acute Stroke Trial and the International Stroke Trial. Neuropsychiatric disorders are common after stroke, including depression, anxiety, agitation, mania, apathy, emotional lability, psychosis, and fatigue (Table 147. Noncognitive neuropsychiatric disorders are distressing to patients, families, and caregivers in the poststroke period, and can significantly interfere with rehabilitation efforts following a stroke [1]. Moreover, these disorders have been shown to be associated with increased morbidity in the poststroke period. Despite their high prevalence and association with increased morbidity, these disorders remain underrecognized by health care professionals and may not always be adequately treated. We present the definition, clinical diagnosis, causes, and treatment of three of the most severe neuropsychiatric complications of stroke, i. Common medications used for the treatment of the neuropsychiatric complications of stroke are summarized in Table 147. In one study of 301 patients who have had a stroke, major depression was present in 20% of the patients and minor depression (defined by the presence of more than two but less than five depressive symptoms) occurred in another 20% of patients [4]. Studies suggest that the mean duration of poststroke depression is 9 months, with cortical lesions showing a longer duration of poststroke depression than subcortical and brainstem lesions. Poststroke depression is associated with worse functional outcomes and increased mortality after a stroke, even after correcting for other variables such as age, gender, and stroke location [3]. Patients with minor or major poststroke depression have significantly less recovery in motor and language functions at 2 years compared with patients who have had a stroke with no post-stroke depression, and who had comparable stroke care. Cognitive impairment is more common in stroke patients with depression, particularly in association with left-hemisphere lesions. Given the high prevalence of stroke and its association with increased morbidity and mortality, current guidelines recommend that all patients be screened for mood disorders, including depression, within 6 weeks of a stroke [1]. In patients whose strokes result in significant motor or language deficits, a distinction between a normal adjustment reaction and a major depressive disorder should also be made. Several brief screening tools for depression have been validated in stroke cohorts and are available for use in clinical settings. These include the Beck Depression Inventory, the nine-item Patient Health Questionnaire, the Center for Epidemiologic Studies Depression Scale, the Hospital Anxiety and Depression Scale, and the Hamilton Depression Rating Scale. These tools are helpful in identifying patients who would benefit from more detailed neuropsychiatric evaluations and follow-up. Fatigue, psychomotor retardation, sleep, and appetite disturbance may represent somatic rather than neuropsychiatric complications of stroke; therefore, clinical judgment is often needed to assess whether these symptoms are indicative of poststroke depression. Furthermore, assessment of depression may be particularly challenging in the presence of aphasia, loss of vocal inflection, impaired attention, or altered facial expression patterns that may mask or mimic the symptoms of depression. Observer-rated screening tools, such as the Stroke Aphasia Depression Questionnaire and the Depression Intensity Scale Circles, may be particularly helpful in these cases.
Time lapse before drug works: Improvement may be seen in 4 weeks antibiotic 933171 order tri azit cheap, but it may take 3 months for maximum benefits. Prolonged use: Visit the doctor regularly to see if the drug continues to be effective and to monitor your blood and platelet counts. Driving, piloting or hazardous work: Avoid if you feel dizzy, otherwise no special problems expected. These include bacterial, viral and fungal infections that can be serious, possibly fatal. Danger increases if you drink alcohol or take medicine affecting alertness and reflexes, such as antihistamines, tranquilizers, sedatives, pain medicine, narcotics and mindaltering drugs. Consult doctor if any of the following symptoms occur: decreased urination, dizziness or lightheadedness, dryness of mouth, increased thirst, wrinkled skin. They may contain salicylates* and can lead to increased risk of side effects and overdose. To help the medicine reach your stomach faster and to prevent throat irritation, stay upright for 30 minutes after you take it. Osteoporosis and osteopenia are progressive diseases in which bone breakdown occurs faster than bone formation. Infrequent: Mild bone or muscle pain, nausea, diarrhea, constipation, gas, leg cramps, bloated feeling, anxiety, depression, throat pain or irritation, mild heartburn, swallowing difficulty, headache, weak muscles. Prolonged use: Visit your doctor regularly to determine if the drug is continuing to control bone loss. After stopping the drug, it still remains in the body bound to the bone for as long as 10 years in some patients. Infrequent: Injection site discomfort or redness, nausea, headache, stomach cramps, dizziness. Rare: Leg cramps, light-headedness when rising after sitting or lying down, syncope (fainting), vertigo. Over age 60: No special problems expected, but caution should be used in the elderly. Breastfeeding; Lactation; Nursing Mothers: Normally not used in premenopausal women. Teriparatide works effectively with certain other drugs for osteoporosis because the drugs work by different mechanisms. May also be used for lines and wrinkles in the forehead, around the eyes, in the lower face area and the neck. What drug does: It paralyzes, weakens or relaxes the injected muscle by blocking the release of a chemical that normally signals the muscle to contract or tighten. Time lapse before drug works: Improvement may be seen in 1-3 days and lasts up to 3-6 months.
The analysis of the skeletonized images demonstrated increased branch density in diabetic animals treatment for glaucoma dogs generic 100mg tri azit with visa. Increased vascular endothelial growth factor and reactive oxygen and nitrogen species signaling appears to be the underlying mechanism. Cerebrovascular Function in Diabetes Cerebrovascular function is also affected negatively in diabetes. An important property of the cerebral vasculature is its autoregulatory capacity, mostly due to myogenic behavior of the vascular smooth muscle in arterioles. Cerebral vessels constrict and dilate in response to increasing or decreasing pressure, respectively. Myogenic tone is increased in early diabetes and as animals age, they lose this ability, which limits the ability of the cerebrovasculature to regulate blood flow, rendering the brain more vulnerable to changes in pressure. The use of different models of diabetes with varying disease severity also provided very valuable information with regard to infarct size, hemorrhagic transformation, and edema and their relevance to functional outcomes. Again, there is more hemorrhage formation and edema than found in control animals. Despite the fact that these rats have smaller infarctions, their neurologic deficit is greater suggesting that the infarct size is not the sole determinant of poor outcomes in diabetes [1]. As discussed under "cerebrovascular structure" in the previous section, these animals display extensive cerebrovascular remodeling and neovascularization [1]. It is highly likely that newly formed immature vessels are susceptible to reperfusion injury and bleeding causing hemorrhagic transformation of the infarct. Diabetes mediates early vascular dysfunction triggering changes in cerebral blood flow, which in turn stimulates dysfunctional neovascularization and neurovascular remodeling. These pathological changes in the cerebrovasculature create a microenvironment that renders the brain more susceptible to ischemic stroke and cognitive impairment. Studies showed that neuronal plasticity is greatly blunted in type 1 diabetes [10]. Coinciding with these changes, sensorimotor recovery as well as cognitive function is significantly impaired [11]. Metformin treatment started after stroke provides glycemic control and also prevents the massive loss of vascular tissue, in part by regulation of the redox signaling that promotes endothelial cell death. Cognitive impairment has been demonstrated in both type 1 and type 2 models of diabetes [12]. Cerebral myogenic reactivity and blood flow in type 2 diabetic rats: role of peroxynitrite in hypoxia-mediated loss of myogenic tone. Diabetes impairs cortical plasticity and functional recovery following ischemic stroke. Two of the most detrimental diseases related to aged cerebrovascular dysfunction are stroke and vascular dementia. Aging is associated with changes to the immune system, neural networks, and vascular regulation. Vascular compliance is impaired with aging, which may contribute to vascular dementia. Damaged organs can release a host of inflammatory factors that compromise the cerebrovasculature. Comorbid diseases associated with peripheral organ dysfunction enhance the inflammatory response to brain damage. Endothelial dysfunction can occur very early in the disease and gradually lead to changes in cerebral blood flow that creates a hypoxic environment. Thus early interventions to improve cerebrovascular function have the potential to limit devastating cerebral complications of diabetes. The independent effect of type 2 diabetes mellitus on ischemic heart disease, stroke, and death: a population-based study of 13,000 men and women with 20 years of follow-up. Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: a systematic overview. Discount tri azit 250 mg on-line. AS Biology Unit 3- Antimicrobial properties of mint and garlic practical.
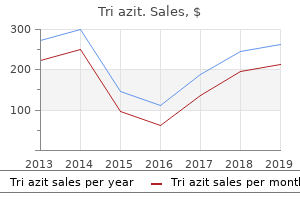
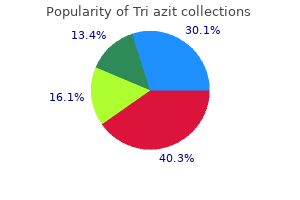
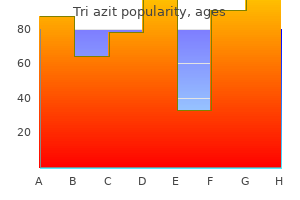
|