Urispas"Order urispas 200 mg with amex, muscle relaxant orange pill". By: B. Moff, M.B. B.CH. B.A.O., M.B.B.Ch., Ph.D. Assistant Professor, Texas Tech University Health Sciences Center Paul L. Foster School of Medicine In an insurance-based system the woman may feel that the operation is her right because she has paid for it in her insurance premiums muscle relaxant in renal failure 200mg urispas overnight delivery. Her insurer may refuse to pay for her to have a second opinion or to come back at an interval to discuss the matter on a second occasion with her gynaecologist. The doctor may well have been running behind the clock by the time the interview takes place and there may be precious little time. Thus, the discussion often takes place when there are pressures to reach a decision swiftly. Take for example, fibroid-related complaints which now account for 20% of appointments in benign gynaecology clinics. Patients may have multiple symptoms and fail to appreciate that no procedure will address all the items on their list. If she has come determined to get the operation she is likely to describe those symptoms in emphatic if not exaggerated terms. The crux is that the dice are loaded in favour of the woman getting the specific surgical procedure appropriate to the symptoms that she describes. In cases that I am instructed to defend, the doctors are often criticised for a failure to mention a risk that would have led the patient to choose not to undergo the operation. The implication is that the doctor has a vested interest in performing the procedure. He who corrects the in growing toe-nail receives a few shillings: he who cuts your inside out receives hundreds of guineas, except when he does it to a poor person for practice. But we take good care not to make the hangman and the housebreaker the judges of that. But we do make the doctor the judge, and fine him anything from sixpence to several hundred guineas if he decides in our favour. I cannot knock my shins severely without forcing on some surgeon the difficult question, "Could I not make a better use of a pocketful of guineas than this man is making of his leg And the 23 413 Section E Aspects of Multidisciplinary Care in Gynaecology guineas would make all the difference in the world to me just now. My wife-my pretty ones-the leg may mortify-it is always safer to operate-he will be well in a fortnight-artificial legs are now so well made that they are really better than natural ones-evolution is towards motors and leglessness, etc. That he has the sort of single minded determination exhibited in the YouTube comic video Orthopaedics vs. The reality is quite the reverse: many of the patients who attend a gynaecology out-patient clinic have come determined to get the operation that they have already decided is their right. Indeed in the case of gynaecological oncology, a refusal to accept a radical surgical solution is not likely to diminish the need for medical advice. The surgeon should offer to refer the patient to the medical oncologists just as would have happened if they had previously undergone surgery. A patient will have capacity if she is able to understand the information she is given and to handle that information so as to be able to take her own decision. In English law this involves considering whether the patient has granted someone a lasting Power of Attorney to take decisions on her behalf and, if that is not the case making enquiries of members of the family or others to ascertain what her wishes would be likely to be, before acting as he sees would be in her best interests. You should discuss with them their condition and treatment options in a way they can understand and respect their right to make decisions about their care. You should see getting their consent as an important part of the process of discussion and decision making, rather than something that happens in isolation. Plainly, if a patient decides not to undergo a procedure that she has been offered that will be an end of the matter and it may well be a thoroughly good thing. In the case of a benign condition, such as fibroids, endometriosis or urinary stress incontinence, such a decision may well be no more than the result of re-assessing her own symptomatology in the light of the information that she has been given by the doctor about the realistic prospects of a complete relief of her symptoms as a result of surgery. The patient is entitled to refuse to consent to treatment in the words of Lord Donaldson for good reason, bad reason or no reason and it will behoves a doctor who has not experienced the symptoms of which this patient complains to seek to second guess her decision. A refusal to accept a therapeutic intervention when there are excellent prospects of a cure is likely to puzzle the gynaecological oncologist where the negative decision appears to be fraught with far more hazard. In self-defence, the doctor must make the clearest clinical Demands for Positive Intervention Sometimes the patient demands a positive intervention that the doctor believes not to be in her best interests.
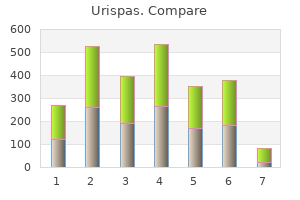
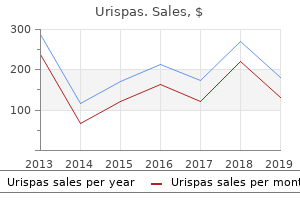
Robotic-assisted spasms lower back discount urispas american express, laparoscopic, and abdominal myomectomy: a comparison of surgical outcomes. High recurrence rate of uterine fibroids on transvaginal ultrasound after abdominal myomectomy in Japanese women. Optimal timing and mode of delivery after cesarean with previous classical incision or myomectomy: a review of the data. The World Health Organisation classifies ovarian tumours depending on their precursor origin (Table 10. This can be broadly divided into epithelial tumours, sex-cord stroma tumours and germ-cell tumours; all of which can either be benign or malignant or borderline in the case of epithelial cell. Ovarian cysts may be asymptomatic and found incidentally clinically or by ultrasound scan. Alternatively they may cause pain or discomfort, or present with bladder or bowel disturbance if they are large and exert pressure on surrounding viscera. Ovarian cyst accidents or torsion may present acutely with severe abdominal pain, which may radiate to the thigh, and are often associated with nausea and vomiting. Functional cysts: the physiological process of ovulation can lead to the development of ovarian functional cysts but these are not pathological. Functional cysts arise from a Graafian follicle (the dominant follicle in the menstrual cycle) or a Table 10. There are reports of functional cysts being >30 cm in diameter,3 and if they are causing symptoms then surgical removal may be necessary. However, because of their tendency to regress the management of a simple cyst in an asymptomatic patient should be conservative with ultrasound follow-up. Iatrogenic cysts will be present after ovulation induction therapy and can reach a significant size in ovarian hyperstimulation syndrome (see Chapter 12). Surgical intervention is only required for serious complications, namely rupture and haemorrhage or torsion. Smaller cysts will be palpable on bimanual examination by the presence of fullness in either adnexa. Positive examination findings will be easily missed if the patient is overweight or there is patient discomfort during the examination. A transvaginal approach has been shown to improve sensitivity when compared Granulosa-stromal cell Steroid cell tumours Sertoli-stromal cell Germ-cell Mature teratoma Thyroid tumour Dermoid cyst Struma ovarii Section B Benign Conditions: the Cervix, Vagina and Vulva, Uterus, Ovaries and Fallopian Tubes Table 10. Diagnostic laparoscopy may be useful for further evaluation of a suspected cyst on occasion, and laparoscopy for pelvic pain or infertility may result in the finding of a previously unsuspected ovarian cyst. The benefits have been well demonstrated including increased patient satisfaction, shorter hospital stay and recovery, quicker return to work and decreased intra-abdominal adhesion formation. The objectives and surgical techniques are broadly similar to the open approach, and much will depend on the level of expertise of the laparoscopic surgeon. Aspiration of the cyst is generally discouraged, especially in post-menopausal women due to the poor sensitivity of cyst fluid cytology9 and increased risk of cyst recurrence. If the cyst appears benign and the patient is pre-menopausal, it is usually important that healthy ovarian tissue be conserved. It is recommended that a risk of malignancy index be calculated to select women who are at high risk of having a malignant tumour and thus be referred and managed by the appropriate team. If an ovarian tumour is removed and subsequently found to be malignant, it may be necessary to subject the patient to a further abdominal operation for correct treatment and staging. A little traction is usually necessary and any connective tissue passing from the substance of the ovary into the capsule of the cyst can be divided by sharp dissection. The aim is to remove the cyst with the capsule intact although this may be technically difficult especially if the cyst is thin-walled.
Occasionally there is some urinary leakage through the drain but this usually settles without further intervention muscle relaxant india purchase generic urispas line. There are three alternative procedures: 21 Transvesical (Extra-Peritoneal) Repair the bladder is opened extra-peritoneally by a standard retropubic cystotomy approach. The fistula may be elevated by the insertion of a tight intravaginal pack and further steadied by the insertion of a surgical hook. The remainder of the surgical procedure is exactly similar to that employed for a vaginal approach. It may be necessary to insert a ureteric catheter to avoid inclusion of the intramural ureter if this is at risk. When operating through the bladder a continuous suture to the urothelium is acceptable. This is rather more haemostatic, and it is important to avoid clot retention after surgery. Polyglactin sutures are used throughout both for the closure of the fistula and for closure of the cystotomy. In this technique the peritoneal cavity is opened and the plane between the bladder and vagina entered to expose the fistula track. In the presence of adhesions this route is not to be recommended as there is significant risk of further damage to the bladder outside the fistula when the anatomy is grossly distorted. This approach, however, can be combined with hysterectomy if appropriate (see vesico-uterine fistula). Combined Transperitoneal Transvesical Approach (Swift-Joly) this is probably the easiest technique to apply for a relatively straightforward post-hysterectomy fistula. The bladder is opened in the mid-line at the vault and bivalved in the median 382. If, however, mobilisation of the bladder is dif cult a cystotomy should be performed. Suf cient greater omentum can usually be mobilised to reach the pelvis if it can be detached from the anterior surface of the transverse colon and then separated in the supracolic portion from the greater curve of the stomach, following ligature and division of the left gastro-epiploic artery. A vascular pedicle based on the right gastro-epiploic artery remains to preserve viability. A fistula that involves the bladder neck should be reinforced to preserve continence and the insertion of a Martius graft may be advantageous. Even a relatively sparse omentum can be mobilised by careful dissection from its attachment to the transverse colon. The left gastro-epiploic artery is divided, together with short communicating vessels to the stomach, to allow mobilisation of the gastro-epiploic arcade based on the right gastro-epiploic artery. Total Urethral Loss-Reconstruction (a) Dennis Browne (modified by Chassar Moir 1964): If there is sufficient vaginal epithelium it may be possible to mobilise distal vaginal wall so as to bury a strip of epithelium as in the operation for male hypospadias. Suprapubic drainage must be maintained long enough to allow the epithelium to grow round to form a tube. The main difficulty is that there may be insufficient healthy distal vagina other than epithelium over scar tissue, from which to fashion the new urethra. A modified Martius graft largely overcomes this problem and may reduce the problem of stress incontinence. The surgical management of ureteric fistula uses the techniques utilised for acute ureteric injury or deliberate resection. Repair is best achieved by the abdominal route-the Swift Joly combined approach is appropriate (see above). It may be necessary to dilate the cervix from below if granulations from the posterior uterine wall are occluding the cervical canal. A U-shaped incision is made and the tissues on each side of the incision carefully mobilised. Operative mortality is uncommon but associated with Gramnegative septicaemia, especially in immunocompromised patients. Inadvertent fistula enlargement can complicate closure, and just occasionally a fresh injury may be perpetrated. Failure may also be associated with non-recognition of intrinsic pathology, associated abscess or foreign body. The ureter is at risk from inclusion in a suture when in close proximity to a fistula.
Prospective clinical trials are underway to assess the validity of a screening programme muscle relaxant addiction order urispas 200 mg amex. Tumour involving one or both ovaries with peritoneal implants outside the pelvis and/or positive retroperitoneal or inguinal nodes. Tumour is limited to the true pelvis but with histologically proven malignant extension to small bowel or omentum. Tumour grossly limited to the true pelvis with negative nodes but with histologically con rmed microscopic seeding of abdominal peritoneal surfaces. Tumour of one or both ovaries with histologically con rmed implants of abdominal peritoneal surfaces none exceeding 2 cm in diameter. Abdominal implants greater than 2 cm in diameter and/ or positive retroperitoneal or inguinal nodes. Decision for Surgery Once the diagnosis has been either suspected or made then the decision as to who should operate, when and where needs to be taken. Either primary surgery will be decided upon or neoadjuvant chemotherapy usually followed by a delayed laparotomy. The surgery should be undertaken by a trained abdomino-pelvic surgeon with an understanding of the natural history of the disease as well as its pathology. This surgeon should be a gynaecological oncologist and there is good evidence to show that the outcome for women with ovarian cancer will be better if this is the case. These specialists optimise surgical debulking and resection of tumour, also minimising the risk of a faecal diversion. Whilst the surgical gynaecological oncologist is the most important member of the multidisciplinary team, working closely with radiological and medical oncological colleagues is essential to determine (a) the most appropriate time for surgery to be carried out and (b) the most suitable chemotherapy for treatment of primary disease and for recurrence as and when it occurs. Decision for Surgery or Neoadjuvant Chemotherapy Surgical resection of tumour (cytoreduction) remains the cornerstone of current treatment for patients with advanced and early stage ovarian cancer. However, when there is widespread disseminated, often small volume, disease optimal resection of tumour may be impossible. It has been accepted for many years that the Pathology Ninety per cent of ovarian tumours are epithelial in origin with the majority being serous cystadenocarcinomas. A smaller number are mucinous in origin, endometrioid or of clear cell morphology. Approximately 5% will be germ cell or gonadal-stromal tumours with a further 5% being secondary tumours from other primary sites including the breast or gastrointestinal tract. Such surgery may include diaphragmatic resection, splenectomy, distal pancreatectomy and liver resection. This may be optimal leaving behind no residual microscopic disease or sub-optimal. Prognosis is directly related to the amount of residual disease remaining after primary surgery. The aim of surgery should however be to remove all macroscopic disease unless it is truly inoperable due to its location, but not due to the inability of the surgeon carrying out the procedure. It is essential that the surgeon is trained in extensive abdominal surgical procedures to carry out these very extensive operations. The first is to fully assess and stage the disease and the second, to carry out a therapeutic procedure, i. Advanced disease or early stage disease with bulky enlarged ovarian masses necessitates a laparotomy through an extended midline incision. On opening the abdomen peritoneal washings should be taken using 300 cc of normal saline instilled into the abdominal cavity and pelvis. If there is no obvious evidence of peritoneal disease then blind biopsies should also be taken from the pelvis and paracolic gutters. Any suspicious nodules should be excised and biopsied and then appendicectomy carried out for mucinous tumours. The whole of the abdomen and pelvis is explored from the diaphragm to the pelvic floor. The retroperitoneum is also extensively assessed with the resection of bulky nodes from either the para-aortic region or the pelvis paracolic gutters. This includes not only the pelvic nodes on the side of a primary tumour but also the para-aortic nodes up to and including the level of the renal vessels. Generic urispas 200mg. Top 10 Most Abused Prescription Drugs.
It now has an established role in gynaecological malignancies discussed later in the chapter muscle relaxant metaxalone side effects generic 200 mg urispas with mastercard. Brownian motion of protons is reduced with increasing cellular density/cell membranes and increasing extracellular macromolecules. This reduction of motion is seen as increasing signal intensity on diffusionweighted images. The patient is injected with a gammaemitting labelled tracer and its distribution after a period of time is detected by modified gamma cameras containing scintillation crystals which are read by photomultiplier tubes. However these require superimposition of data acquired retrospectively and normal variations in position and activity of bowel, respiration and cardiac function contribute to correlation errors. It has an increasingly important role in oncology for diagnosis, staging, predicting response to treatment and in the detection of recurrent disease. It utilises biochemical metabolites (commonest 2-deoxy-d-glucose), labelled with beta-emitting radiotracers (18-Fluorine) that are injected intravenously. Both glucose and deoxyglucose enter cells via cell glucose transporters and undergo phosphorylation but while glucose undergoes further enzymatic breakdown, deoxyglucose becomes trapped in intracellular compartments. Cancer cells have increased glucose cell membrane transporters and intracellular phosphorylation enzymes thereby take up and trap more glucose and deoxyglucose than normal cells. The 18Fluoro component undergoes beta decay in the body producing a high-energy positron. Once the positron slows down it produces two gamma rays which are emitted back-to-back and have energy of 511 KeV each. The aim is to provide imageguided, minimally invasive alternatives to traditional surgical and medical procedures in suitable patients. Percutaneous radiofrequency ablation techniques of liver and lung metastases have survival benefits equivalent to surgical metastectomy but are still sparingly used in gynaecological malignancies. Over the past decade software-based algorithms have been developed 49 Section A Introduction, Anatomy, Pre-op. Criteria for characterising malignant masses on ultrasound have been described and include masses larger than 10 cm, the presence of soft tissue nodules (soft tissue components) and vegetations, thickened irregular walls, thickened nodular septae, presence of ascites and peritoneal nodules. Its role has been formally defined by the female imaging subcommittee of the European society of urological radiologists. In particular, two large submucosal broids are seen extending into the endometrial cavity and distorting the cavity (dashed arrows). All the broids are demonstrated as vascular enhancing masses thereby suitable for embolisation (arrows). The multiple broids have decreased in size, in particular the sub-mucosal broids which no longer distort the endometrial cavity (dashed arrows). Most of the uterine broids are now avascular and non-enhancing in keeping with a good response following embolisation (arrows). Computed tomography is useful in detecting ascites, pleural effusions, tumour involvement of intra-abdominal viscera, mesentery, peritoneal reflections and omentum. It has better accuracy detecting implants on bowel serosal and invasion of the sigmoid colon, bladder and rectum. Care predictive value in ruling out not only patients with endometrial cancer but also any other endometrial abnormality, such as polyps or hyperplasia. The depth of myometrial invasion is an important prognostic factor in endometrial cancer, the incidence of nodal metastases increasing sharply from 3% in tumours with no or superficial myometrial invasion to 40% in tumours with deep myometrial invasion. For the detection of deep myometrial invasion the sensitivity and specificity are 83% and 42%, respectively. For the detection of cervical invasion the sensitivity and specificity are 25% and 70%, respectively. Computed tomography is therefore of limited value for local staging and unlikely to affect management in early endometrial cancer.
|