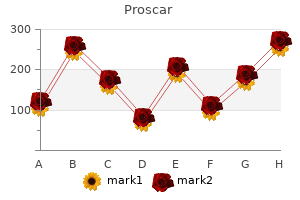
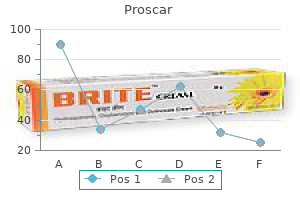
Proscar"Order 5 mg proscar amex, androgen hormone excess". By: O. Daro, M.A., M.D. Co-Director, University of Michigan Medical School The ability to improve constipation while preserving analgesia compared with use of oxycodone alone was confirmed in a group of cancer patients (Ahmedzai et al androgen hormone zits cheap proscar line. These studies did not show an excess of opioid withdrawal effects, perhaps as a result of the lower peak of naloxone absorption achieved through use of the sustained-release mechanism rather than the immediate-release formulation employed in previous studies. It might be noted that the low oral bioavailability of naloxone depends on rapid metabolism by the liver: in hepatic impairment blood levels can be very much greater. Patients with impaired liver function were excluded from trials of the oxycodone/naloxone combination. Clinical manifestations and diagnostic considerations Diarrhoea persisting for over 3 weeks is said to be chronic and is often linked to serious organic disease. Most diarrhoea is acute, lasting only a few days, and is generally the result of gastrointestinal infection (Box 10. However, the commonest cause of diarrhoea in palliative medicine is an imbalance of laxative therapy (Twycross and Lack, 1986b). This particularly occurs when laxative doses have been increased to clear a backlog of constipated stool. Meanwhile the diarrhoea may be distressing, especially if it leads to faecal incontinence. A variety of other common drugs can also precipitate diarrhoea, either commonly, as in the case of antacids and antibiotics, or idiosyncratically, as in the case of non-steroidal anti-inflammatory agents or iron preparations. Those receiving enteral feeding appear particularly prone, sorbitol being more than twice as likely to be the cause of diarrhoea as the feed itself (Edes et al. Malignant intestinal obstruction and faecal impaction are the next most common causes of diarrhoea in this patient group. Complete intestinal obstruction produces intractable constipation, but partial obstruction may present with either diarrhoea or alternating diarrhoea and constipation. Faecal impaction results in fluid stool leaking past the mass, often with anal leakage or incontinence. In elderly patients hospitalized for non-malignant disease, faecal impaction can account for 55% of instances of diarrhoea (Kinnunen et al. Many disease-modifying medication used in the palliative management of advanced cancer can cause diarrhoea. Additionally, almost all of the recently developed small-molecule-targeted therapies cause Diarrhoea Diarrhoea is the passage of frequent loose stools with urgency. Radiotherapy involving the abdomen or pelvis is liable to cause diarrhoea, with a peak incidence in the second or third week of therapy and continuing for some time after cessation of the course. Damage to intestinal mucosa by radiation results in the release of prostaglandins and the malabsorption of bile salts, both of which increase peristaltic activity. Uncommonly, another iatrogenic cause of diarrhoea relevant to palliative care is coeliac plexus blockade, which can be associated with the onset of profuse, long-lasting watery diarrhoea. This possibly results from anatomical variations in the innervation of the gut so that in certain individuals interruption of the coeliac plexus has an excessive influence on bowel activity (Dean and Reed, 1991). A different type of malabsorption that can be seen in palliative care patients treated with antibiotics, or as a complication of gut infection such as Clostridium difficile, is lactose intolerance secondary to changes in the intestinal flora. This will gradually correct itself but meanwhile a lactose-free diet produces prompt resolution of the diarrhoea (Noble at al. If less than 100 cm of terminal ileum is removed, fat malabsorption generally does not occur, as the liver can compensate for the increased biliary loss.
The use of neomycin prostate exam procedure cheap 5mg proscar with mastercard, metronidazole, ampicillin and, more recently, rifaximin have been described (Festi et al. Pathogenesis of cholestatic itch: old questions, new answers, and future opportunities. Opiate antagonist therapy for the pruritus of cholestasis: the avoidance of opioid withdrawal-like reactions. Patient-reported outcomes in palliative gastrointestinal stenting: a Norwegian multicenter study. Review of the final report of the 1998 Working Party on definition, nomenclature and diagnosis of hepatic encephalopathy. The PleurX Peritoneal Catheter Drainage System for Vacuum-Assisted Drainage of Treatment-Resistant, Recurrent Malignant Ascites. Mobilization of malignant ascites with diuretics is dependent on ascitic fluid characteristics. Summary At present, given the relative lack of evidence for any of the medical interventions described, it is imperative that any individual presenting with hepatic encephalopathy is, if appropriate given the context of the associated disease process, intensively investigated for precipitating factors. If no precipitating factors are identified or symptoms are persistent, then antibiotics such as neomycin or particularly rifaximin, if available, should receive a trial of therapy. The care of individuals with covert hepatic encephalopathy continues to be a worthy subject of debate. Palliation of malignant biliary obstruction: a prospective trial examining impact on quality of life. Symptom relief and quality of life after stenting for malignant bile duct obstruction. Effect of endoscopic stenting of malignant bile duct obstruction on quality of life. To stent or not to stent: an evidence-based approach to palliative procedures at the end of life. The use of midazolam to treat itching in a terminally ill patient with biliary obstruction. The diagnosis of subclinical hepatic encephalopathy in patients with cirrhosis using neuropsychological tests and automated electroencephalogram analysis. The development of clinical guidelines on paracentesis for ascites related to malignancy. Denver peritoneovenous shunts for the management of malignant ascites: a review of the literature in the post LeVeen Era. Fearon Introduction to aetiology, classification, assessment and treatment of the anorexia-cachexia syndrome the anorexia-cachexia syndrome is a complex multidimensional problem and, until recently (Evans et al. This had led clinicians to feel that perhaps it was not worth trying to grapple with the difficult problem of assessment and treatment of patients with cachexia. Recent progress in our understanding of the underlying biology and the development of new biological therapeutic targets has led to a new era of hopeful optimism. The aim of this chapter is to resolve some of these issues and provide (a) the reader with some background principles to classification, (b) a simple approach to patient assessment and a robust algorithm for basic multimodal treatment, and (c) an overview of the evidence base for different pharmacological interventions. The common feature of cachexia is that it is not possible to completely reverse the syndrome with conventional nutritional support. Whilst undoubtedly there are common mechanisms of wasting in each of these conditions, there are many unique aspects which are too complex to explore in a single chapter. It is hoped that the principles outlined will provide a platform on which to build an approach for other groups of patients. Before approaching classification and therapeutics, it is useful to have some understanding of the pathophysiology of cachexia as these principles should underpin the logic behind the clinical management of patients. Cachexia is characterized by a negative energy and protein balance driven by a variable combination of reduced food intake and abnormal metabolism. Thus it is important to assess and manage actively both food intake and abnormal metabolism in all patients. Cancer cachexia may be considered initially an adaptive response to access body stores of energy and protein. Mobilization of skeletal muscle and adipose tissue is a highly organized response. Inflammation is widely agreed to be a unifying mechanism for the entire cluster of sickness behaviours (asthenia, increased slow wave sleep, mood alteration, lethargy, depression, anorexia, fever, anhedonia, cognitive impairment, hyperalgesia, and decreased social interaction), including loss of fat and muscle.
This is evidenced by the prevalence of chronic post-surgical pain in patients who have undergone mastectomy without accompanying axillary node dissection and with documented sparing of the intercostobrachial nerve (Carpenter et al prostate cancer untreated life expectancy discount proscar 5mg fast delivery. It has been well documented that adjunctive radiation in breast cancer patients increases their risk of developing a chronic pain syndrome. The most common cause of pain in this setting includes radiation-induced plexopathy, especially brachial plexopathy. Brachial plexopathy is often heralded by numbness and paraesthesias of the hands and fingers, followed by weakness and increasing pain. It is thought to result from a combination of direct cell damage from ionizing radiation and progressive ischaemic changes which may lead to fibrosis surrounding the nerves of the brachial plexus, fibrous thickening of the neurilemmal sheath, demyelination, and fibrous replacement of nerve fibrils (Qayyum et al. Other less common causes include osteoradionecrosis of the chest wall, fractures, and secondary malignancies (Paice, 2011). The most common cause of peripheral neuropathy in the breast cancer population is the use of chemotherapeutic agents. Peripheral neuropathy is often the dose limiting side effect of these agents (Reyes-Gibby et al. It is believed to be secondary to intercostal nerve damage as well as suboptimal control of acute pain in the immediate postoperative period. Aggressive rib retraction may also contribute by leading to costovertebral and costochondral dislocation. The syndrome is characterized by significant burning pain with other associated neuropathic features postoperatively with a very slow resolution in the following months and years. One study found that approximately 30% of patients continued to report pain at 5 years post thoracotomy with no significant decrease in pain intensity (Dajczman et al. Preoperative epidural analgesia has been shown to be more effective at reducing the incidence and intensity of the resultant chronic pain than postoperative epidural analgesia (Obata et al. Haematological/stem cell transplantation Haematological malignancy survivors are at an increased risk of developing chronic pain syndromes due to several potential treatment related complications. These pain syndromes are of particular concern in the setting of stem cell transplantation, given the treatment intensity. Patients may experience significant bone pain as a result of prolonged steroid therapy as treatment for graft-versus-host disease. Haemorrhagic cystitis is another painful condition, which can result from certain conditioning regimens, especially those containing cyclophosphamide and total body irradiation. The immune-suppressing calcineurin inhibitors used prophylactically post stem cell transplant to prevent graft rejection. Carbamazepine is thought to exert its analgesic effect through the reduction of conductance in sodium channels and may have a particular role in the management of trigeminal neuralgia. Gabapentin and pregabalin are similar in their mechanism of action, which appears to be delivered via interaction with the 2- protein subunit of voltage-gated calcium channels. Pregabalin displays linear absorption as opposed to gabapentin, giving it a more predictable dose response range and a generally faster time to therapeutic titration. The efficacy of other anticonvulsants for neuropathic pain has not been reliably established in clinical trials. They are mostly used in association with opioids for musculoskeletal pain; however they are not viable options for long-term treatment due to side effects. Treatments Despite numerous advances in the course of the last several years, the management of chronic pain in cancer survivors is often suboptimal, secondary to the complex neurophysiology of many chronic pain syndromes and a relative paucity of education and resources within many oncological settings. It requires an interprofessional approach that details a comprehensive assessment with ongoing reassessment to guide the implementation and integration of pharmacological and non-pharmacological measures. This facilitates the elucidation and revision of the pain source, alteration of the perception of pain, and inhibition of pain transmission to the central nervous system (Ferrer-Brechner et al. Its role in the management of neuropathic as well as nociceptive pain has been confirmed in several clinical trials (Eisenberg et al. Though morphine remains the most widely used opioid, there is presently no evidence to suggest that one opioid is better than another as a first-line agent. Opioid therapy can be administered through several routes, including oral, transdermal and, most commonly, parenteral.
Bladder outlet obstruction from clots can lead to urosepsis prostate cancer freezing treatment generic 5mg proscar with amex, bladder rupture, and renal failure. Clot evacuation can be performed at the bedside by carefully placing a large, stiff-walled haematuria catheter. After clot evacuation, if haematuria persists, a three-way catheter can be inserted and continuous bladder irrigation with saline can be started. All clots must be removed before continuous irrigation is started to avoid over distention and bladder rupture. The patient should be vigorously hydrated using oral and/or intravenous fluids to keep clots from reforming. If clot evacuation is unsuccessful with this approach, the patient should undergo cystoscopy with clot evacuation and consideration of treatments previously described, including fulguration and instillation/injection of agents. Last-resort options include urinary diversion (prevents urine urokinase from coming into contact with the fragile haemorrhagic mucosa) and radical cystectomy (Zebic et al. Bleeding oesophageal varices Current therapies and recommendations for the management of oesophageal and gastric variceal haemorrhage from advanced liver disease are published elsewhere (Garcia-Tsao et al. When endoscopy is used, variceal ligation appears to be generally preferred over sclerotherapy (Garcia-Pagan and Bosch, 2005; Garcia-Tsao et al. A meta-analysis showed superiority of endoscopic (sclerotherapy or variceal ligation) plus pharmacological (octreotide, somatostatin, vapreotide) therapy over endoscopic therapy alone (Banares et al. For heavier bleeding, haemostatic surgical dressings will provide rapid haemostasis and can be left on the wound and covered with an appropriate dressing. A number of other options are available and these are described above and elsewhere (Grocott, 2000; McDonald and Lesage, 2006). Conclusion Bleeding in the palliative care setting may have a variety of causes and clinical presentations. A large number of treatment modalities, local and systemic, are available to address bleeding and massive haemorrhages. The large majority of evidence in support of these modalities, however, is based on case reports, case series, and expert opinion, with only a small number of large randomized studies. Selecting between the different modalities is therefore seldom guided by comparative studies between the modalities. A number of factors need to be considered when selecting between modalities and the overall care approach. These include patient prognosis and expected survival, access to modalities, quality of life, functional status, and ultimately goals of care and patient wishes. A comprehensive review of topical hemostatic agents: efficacy and recommendations for use. Aerosolized vasopressin is a safe and effective treatment for mild to moderate recurrent hemoptysis in palliative care patients. The use of crisis medication in the management of terminal haemorrhage due to incurable cancer: a qualitative study. Management of terminal hemorrhage in patients with advanced cancer: a systematic literature review. Oxidized cellulose dressings for persistent bleeding from a superficial malignant tumor. For many terminally ill people, intimate and sexual moments are a vital aspect of their life, providing a sense of connectedness and assisting the person to explore and find meaning to living, dying, and death (Rothenberg and Dupras, 2010). Entering the palliative phase of any disease frequently results in a reappraisal of life priorities and relationships in the remainder of life. This has the potential to directly impact the manner in which a person connects at the deepest level with a significant other, at a time when chronic and debilitating illness may precipitate a longing for intimate touch and communication. Sexual expression through all of life, but particularly during end-of-life phases, provides a vital form of communication, reassurance, tenderness, and validation of self when grappling with the vulnerability of changing health and wellness (Lemieux et al. Gianotten challenges health professionals to consider that sexual and intimate moments provide a welcome respite and distraction from all that is going as death approaches (Gianotten, 2007). Yet few health professionals view patients in their care as sexual beings and if they do, they struggle to know what and how to raise the topic of sexuality and intimacy within their clinical roles (Hordern and Street, 2007a, 2007b; Gianotten and Hordern, 2011). The following chapter will: has been a reassuring shift in recent cancer and palliative care literature from a traditional, medicalized, and functional focus on patient sexuality, where the emphasis has remained on rates of penetration and orgasmic responses, strength of erections, libido, and menopausal status (Schover, 2005; Miles et al. Order genuine proscar on-line. #NoShaveTODAY Raises Millions For Men’s Health But Carson Daly Wants A Shave | TODAY.
|