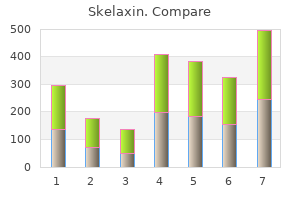
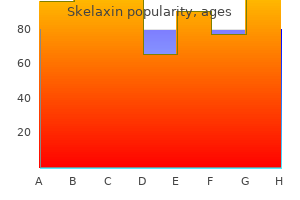
Skelaxin"Skelaxin 400mg for sale, spasms above ear". By: C. Murak, M.A., M.D., Ph.D. Clinical Director, University of Arizona College of Medicine – Tucson Hardy performed the first human lung transplant in 1963 muscle relaxant you mean whiskey skelaxin 400mg low price, although the patient lived only 18 days. These early lung recipients, however, were plagued History Heart Transplants Indications. The most common diagnosis leading to a heart transplant is ischemic dilated cardiomyopathy, which stems from coronary artery disease, followed by idiopathic dilated myopathy and congenital heart disease. Pretransplant, both candidates and potential donors are evaluated to ensure their suitability for the procedure. Transplant candidates undergo echocardiography, right and left heart catheterization, evaluation for any undiagnosed malignancies, laboratory testing to assess the function of other organs (such as the liver, kidneys, and endocrine system), a dental examination, psychosocial evaluation, and appropriate screening (such as mammography, colonoscopy, and prostate-specific antigen testing). Once the evaluation is complete, the selection committee determines, at a multidisciplinary conference, whether or not a heart transplant is needed and is likely to be successful. Once a potential deceased donor is identified, the surgeon reviews the status report and screening examination results. In the recipient, a duodenum-to-donor ileum anastomosis and a distal Bishop-Coop ileostomy are constructed to re-establish bowel continuity. Cooper and colleagues soon determined that the high-dose corticosteroids used for immunosuppression were responsible for the frequent occurrence of dehiscence. The combination of high-dose corticosteroids and ischemic donor bronchi was deadly to lung recipients. Cooper, Morgan, and colleagues showed that the bronchial anastomosis could be protected by wrapping it with a vascular omental pedicle, which not only provided neovascularity but also offered a buttress against any partial dehiscence. In fact, the introduction of cyclosporine allowed the success of the first combined heart-lung transplant at Stanford in 1981 (after unsuccessful attempts by Cooley in 1969, Lillehei in 1970, and Barnard in 1981, all of whom used only high-dose corticosteroids for immunosuppression). Suture lines for bicaval anastomosis (a), biatrial anastomosis (b), aortic anastomosis (c), and pulmonary artery anastomosis (d). Once the cross-clamp is removed, the heart is allowed to receive circulation from the recipient and begins to function normally. Inotropic support with isoproterenol, dobutamine, or epinephrine is often required for 3 to 5 days, in order to support recovery from the cold ischemia. But this scenario is becoming very uncommon with the increasing use of mechanical circulatory support for single-ventricle failure. Most of the immunosuppression used is aimed at T cells; however, if the recipient has many preformed antibodies or develops donor-specific antibodies, other strategies (such as plasmapheresis or rituximab) are used to reduce the antibody load. Other immunosuppressive agents can be used, depending on the needs of individual recipients. Recipients are also assessed for any infections, with visual inspection of wound healing and with monitoring of the complete blood count and cultures as needed. Other common early sequelae include drug-induced nephrotoxicity, glucose intolerance, hypertension, hyperlipidemia, osteoporosis, malignancies, and biliary disease. Accelerated coronary artery disease is the third most common cause of death posttransplant (after infections and acute rejection) and the most common cause after the first year. Because of these late complications, most transplant centers continue to perform screening tests and recipient examinations at least annually after the first year. The next most common diagnosis among patients on the waiting list is cystic fibrosis. The average lung transplant candidate requires oxygen (often 4 L/min or more at rest) and has an extensively compromised quality of life, as documented by the results of pulmonary function and 6-minute walk tests. Patient survival rates for heart recipients differ slightly after primary transplants vs. After primary transplants, the patient survival rates at 1, 3, and 5 years are 87%, 79%, and 72%, respectively; after retransplants, the rates are 82%, 67%, and 58%. Early complications include primary graft dysfunction, acute cellular or antibody-mediated rejection, right heart failure secondary to pulmonary hypertension, and infection. Hemodynamic values are monitored to assess early graft function; pharmacologic and sometimes mechanical support is instituted if needed.
Lower placement risks inadequate pain control spasmus nutans discount 400 mg skelaxin, and higher placement may provoke hand and arm numbness. Ropivacaine has less cardiotoxicity than bupivacaine; thus, the potential for refractory complete heart block, in the case of inadvertent intravenous injection, is significantly less with ropivacaine. Combinations of narcotic and topical analgesia are then infused as with the epidural catheter. When properly placed, a well-managed epidural can provide outstanding pain control without significant systemic sedation. In some patients who are having difficulty voiding, it may be possible to avoid Foley catheterization by simply reminding the patient to void on a regular basis. In male patients with voiding difficulty prior to surgery, urinary catheterization may be required. In addition, the use of local anesthetics may cause sympathetic outflow blockade, leading to vasodilation and hypotension often requiring intravenous vasoconstrictors (an -agonist such as phenylephrine) and/or fluid administration. In such circumstances, fluid administration for hypotension may be undesirable in pulmonary surgery patients, particularly after pneumonectomy. Paravertebral catheters provide equivalent pain control with less effect on hemodynamics. Dosing must be titrated to balance the degree of pain relief with the degree of sedation. Oversedated patients are as ominous as patients without adequate pain control, because of the significant risk of secretion retention, atelectasis/pneumonia, and pulmonary aspiration. These concerns are particularly relevant in elderly patients who should be carefully assessed for aspiration risk when ordered for dietary advancement. Proper pain control with intravenous narcotics requires a carefully regulated balance between pain relief and sedation; maximizing the benefits of pain control while minimizing these very real and potentially life-threatening complications. Whether on epidural, paravertebral, or intravenous pain control, the patient is typically transitioned to oral pain medication on the third or fourth postoperative day. During both the parenteral and oral phase of pain management, a standardized regimen of stool softeners and laxatives is advisable in order to prevent severe constipation. The best respiratory care is achieved when the patient is able to deliver an effective cough to clear secretions and results from the commitment and proper training of all involved healthcare providers. The process begins preoperatively, with clear instructions on using pillows (or other support techniques) over the wound and then applying pressure. Postoperatively, proper pain control (as outlined earlier) is essential, without oversedation. Early transition to a chair and to ambulation is the best respiratory therapy and should be strongly encouraged. When available, physical and/ or cardiopulmonary rehabilitation services are vital additional members of the care team. In patients whose pulmonary function is significantly impaired preoperatively, generating an effective cough postoperatively may be nearly impossible. In this setting, routine nasotracheal suctioning can be employed, but is uncomfortable for the patient. A better alternative is placement of a percutaneous transtracheal suction catheter at the time of surgery. This catheter is well-tolerated by most patients and allows regular and convenient suctioning. The most devastating complication after pulmonary resection is postpneumonectomy pulmonary edema, which occurs in 1% to 5% of patients undergoing pneumonectomy and more often after right compared to left pneumonectomy. Clinically, symptoms of respiratory distress manifest hours to days after surgery. Radiographically, diffuse interstitial infiltration or frank alveolar edema is seen. The pathophysiologic causes are related to factors that increase permeability and filtration pressure and decrease lymphatic drainage from the affected lung. Skelaxin 400 mg discount. What is SOMA?. These acquired gene alterations are termed somatic mutations to distinguish them from germline mutations that are inherited from parents and transmitted to offspring muscle relaxant with alcohol order skelaxin online pills. Most of this damage is repaired; however, a small fraction may remain as fixed mutations. Mutation rates increase in the presence of substantial exogenous mutagenic exposures, such as tobacco carcinogens or various forms of radiation, including ultraviolet light. These exposures are associated with increased rates of lung and skin cancer, respectively, and somatic mutations within such cancers often exhibit the distinctive mutational signatures known to be associated with the mutagen. Whether the somatic mutation rate is always higher during this part of the lineage is controversial. The most common class of genomic alterations among the known cancer genes is a chromosomaltranslocation that creates a chimeric gene. Many more cancer genes have been found in leukemias, lymphomas, and sarcomas than in other types of cancer; and these genes are usually altered by chromosomal translocation. Somatic mutations in a cancer genome may be classified according to its consequences for cancer development. The remainder of mutations are "bystanders" or "passengers" that do not confer growth advantage. Each tumor may have dozens to hundreds of genomic alterations, making it critical to determine which alterations are indeed drivers, and potentially better therapeutic targets. The genomic alterations found in a tumor can also change under the selective pressure of a targeted therapy, adding to the challenge of implementing genomically-informed personalized therapy. Most of our information on human cancer genes has been gained from hereditary cancers. In the case of hereditary cancers, the individual carries a particular germline mutation in every cell. Although hereditary cancer syndromes are rare, somatic mutations that occur in sporadic cancer have been found to disrupt the cellular pathways altered in hereditary cancer syndromes, which suggests that these pathways are critical to normal cell growth, cell cycle, and proliferation. Tumor development at a much younger age than usual Presence of bilateral disease Presence of multiple primary malignancies Presentation of a cancer in the less affected sex. Some of the more commonly encountered hereditary cancer syndromes are discussed here. Pie chart shows the percentage of tumors with each potentially actionable alteration. A "one-hit" clone is a precursor to the tumor in nonhereditary cancer, whereas all cells are one-hit clones in hereditary cancer. The rb1 gene product, the Rb protein, is a regulator of transcription that controls the cell cycle, differentiation, and apoptosis in normal development. Interestingly, although most children with an affected parent develop bilateral retinoblastoma, some develop unilateral retinoblastoma. Furthermore, some children with an affected parent are not affected themselves but then have an affected child, which indicates that they are rb1 mutation carriers. These findings led to the theory that a single mutation is not sufficient for tumorigenesis. A "hit" may be a point mutation, a chromosomal deletion referred to as allelic loss, or a loss of heterozygosity, or silencing of an existing gene. Patients with tumors with similar histologies may differ in genetic mutation status and other molecular features B. Cells within the primary tumor can acquire or lose genomic alterations in metastatic sites. Intratumoral spatial heterogeneity: common initiating genomic events usually exist in all tumor cells but additional spatially separated heterogeneous somatic mutations or copy number changes may accumulate. When cells are exposed to stressors, p53 acts as a transcription factor for genes that induce cell-cycle arrest or apoptosis. The polyps usually appear in adolescence and, if left untreated, progress to colorectal cancer. For example, desmoids usually are associated with mutations between codons 1403 and 1578. Better understanding of the genotype-phenotype correlations may assist in patient counseling and therapeutic planning.
A multicenter evaluation of a new continuous cardiac output pulmonary artery catheter system spasms rib cage buy skelaxin 400mg on line. Standard versus fiberoptic pulmonary artery catheterization for cardiac surgery in the Department of Veterans Affairs: a prospective, observational, multicenter analysis. Mixed venous oxygen saturation cannot be estimated by central venous oxygen saturation in septic shock. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock. The effectiveness of right heart catheterization in the initial care of critically ill patients. A cost/benefit analysis of randomized invasive monitoring for patients undergoing cardiac surgery. Effect of pulmonary artery catheterization on outcome in patients undergoing coronary artery surgery. Routine pulmonary artery catheterization does not reduce morbidity and mortality of elective vascular surgery: results of a prospective, randomized trial. Effectiveness of pulmonary artery catheters in aortic surgery: a randomized trial. A randomized, controlled trial of the use of pulmonary-artery catheters in highrisk surgical patients. Impact of the pulmonary artery catheter in critically ill patients: meta-analysis of randomized clinical trials. Trends in the use of the pulmonary artery catheter in the United States, 1993-2004. Prospective Trial of Supranormal Values of Survivors as Therapeutic Goals in High-Risk Surgical Patients. Prospective, randomized trial of survivor values of cardiac index, oxygen delivery, and oxygen consumption as resuscitation endpoints in severe trauma. Maximizing oxygen delivery in critically ill patients: a methodologic appraisal of the evidence. A randomized and controlled trial of the effect of treatment aimed at maximizing oxygen delivery in patients with severe sepsis or septic shock. The validity of trans-esophageal Doppler ultrasonography as a measure of cardiac output in critically ill adults. Noninvasive whole-body electrical bioimpedance cardiac output and invasive thermodilution cardiac output in high-risk surgical patients. Comparison of continuous cardiac output measurements in patients after cardiac surgery. Finapres arterial pulse wave analysis with Modelflow is not a reliable non-invasive method for assessment of cardiac output. Central venous pressure, pulmonary capillary wedge pressure, and intrathoracic blood volumes as preload indicators in cardiac surgery patients. Implications of arterial pressure variation in patients in the intensive care unit. Effect of tidal volume, intrathoracic pressure, and cardiac contractility on variations in pulse pressure, stroke volume, and intrathoracic blood volume. Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Noninvasive muscle oxygenation to guide fluid resuscitation after traumatic shock. Tissue oxygen saturation predicts the development of organ dysfunction during traumatic shock resuscitation. Continuous intra-arterial blood gas and pH monitoring in critically ill patients with severe respiratory failure: a prospective, criterion standard study. Association between use of lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome: a meta-analysis. Multicenter study of noninvasive monitoring systems as alternatives to invasive monitoring of acutely ill emergency patients. Impact of pulse oximetry surveillance on rescue events and intensive care unit transfers: a before-and-after concurrence study. Intracranial hypertension and cerebral perfusion pressure: influence on neurological deterioration and outcome in severe head injury.
|